extended slightly beyond the lesion perimeter. Many of the lesions
resolved almost completely after a single treatment, and
no additional treatment was required. The data are presented
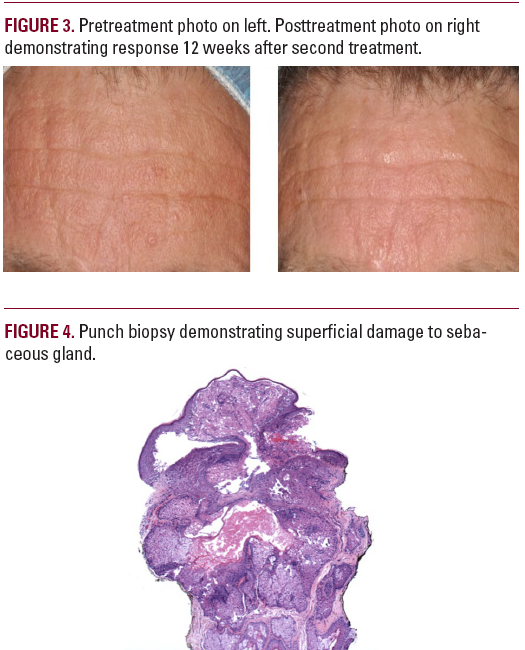
in Table 2. Representative preoperative and postoperative
photographs are noted in Figure 3. Overall, there was a notable
reduction in color, diameter, and height of the lesions.
Crusts were noted by all patients and resolved within 10 days.
The one biopsy showed damage to the sebaceous glands that
extended about 800 µm deep to the surface. The very deep
portion of the lesion (800 µm to 2 mm below the surface) was
unaffected (Figure 4).
DISCUSSION
Sakamoto et al examined 1,720-nm sebaceous gland heating
based on Monte Carlo modeling and ex vivo experiments with
a free electron laser using an ≈8 mm spot.8 Their data suggested
a damage threshold fluence of about 67 J/cm2 for a 50°C
temperature rise based on 100 to 1,000 ms of heating. They also
found about a 1.6 times differential between sebaceous gland
heating and normal skin at selected fluences. Our clinical results
are in line with their preliminary ex vivo results.
However, there are differences in the studies. In their work, a
large spot was used, and normal-sized sebaceous glands were
treated. In our case, only hyperplastic glands were treated. In
these lesions, the glands almost abut the overlying skin surface.

Also, we targeted the lesion with a very small spot vs a larger
spot. We did show selectivity, however, as normal adjacent
skin was unaffected by a range of fluences used in the study.
However, only small increases in dwell time and therefore fluence
resulted in changes in normal skin. Whereas sebaceous
hyperplasia lesions showed coagulation at 50 ms and 3.8 W,
normal skin showed graying only at about 100 ms. The size of
an average sebaceous hyperplasia lesion (about 1-2 mm) has a
thermal relaxation time of about (assuming a spherical geometry)
1 second. Therefore, almost complete thermal confinement
would be expected during the pulse.
The clinical end points with 1,720-nm irradiation differed from
typical clinical end points with other modalities. For example,
with the hyfrecator (probably the most common tool used in sebaceous
hyperplasia treatment), a slight graying at the surface
is noted. With the PDL, purpura is a typical end point, and with
the 532-nm laser, we observe "whitening" as a common end
point. In the later 2 modalities, presumably we are targeting
the Hgb (hemoglobin) that courses through a typical sebaceous
hyperplasia lesion, and indeed those vascular-type sebaceous
hyperplasia lesions respond well to Hgb-specific lasers. Photodynamic
therapy using aminolevulinic acid relies on sufficient
protoporphyrin IX production and adequate light doses to photochemically/
photothermally alter the gland.
The advantage of sebum-selective approaches is a high likelihood
of deeper heating of the gland. Most present methods
only heat the most superficial portions of the gland, resulting
in typical incomplete removal and rapid recurrence. Various
physicians have tried to address this challenge. For example,
Bader and Scarborough used the hyfrecator with a 1-second
application of an epilating needle to heat up lobules without
recurrences.4 Aghassi et al examined the role of PDL in sebaceous
hyperplasia and found specific damage to the blood
vessels.1.Our fiber delivery system and small spot allowed for
precise placement of the beam and, together with the intrinsic
selectivity of 1,720 nm, achieved almost complete clinical
destruction of the lesions without depressions or scarring. By
exploiting the primary differentiating feature of the sebaceous
gland vs normal skin, we achieved complete heating of the






