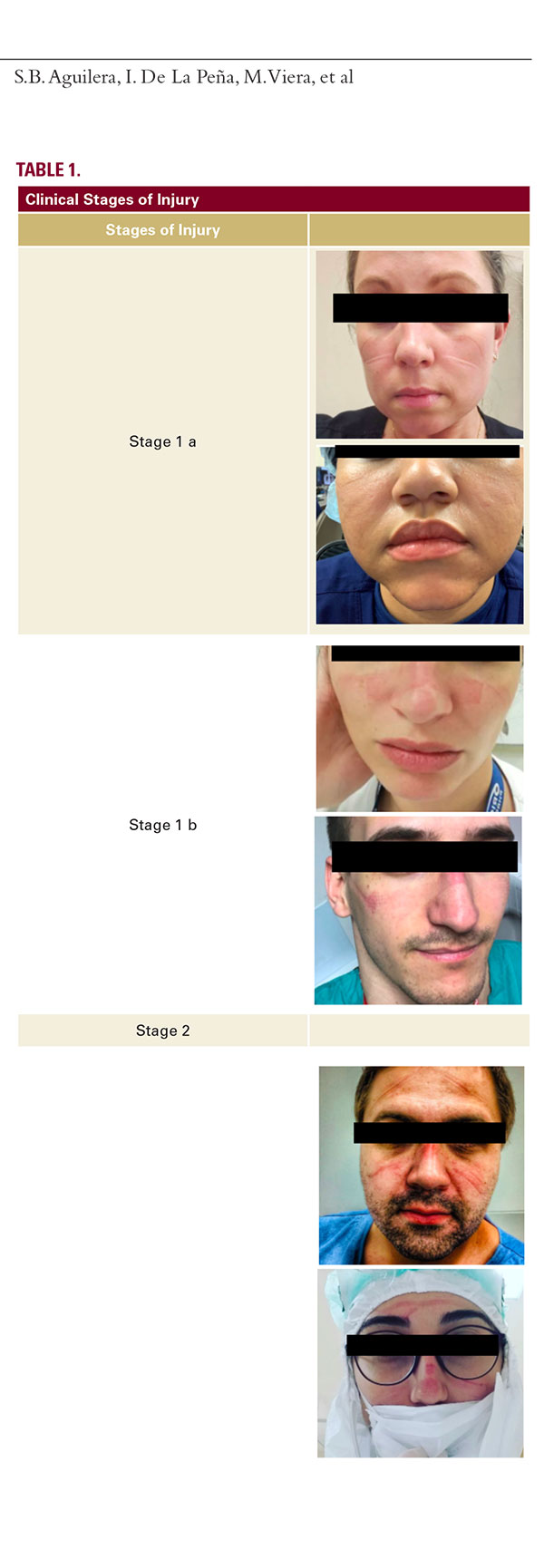
and malar areas that persists more than 24 hours. There is edema and induration of the tissue particularly of the nasal bridge where pain and heat can be experienced. This is related to the use of face masks for more than 6 straight hours of use or everyday compression of the same skin areas.
Stage 2:
The persistent non blanchable erythema is accompanied with shearing lesions because of the increased friction factor. The lesions are characterized by crust formation associated with edema and induration. The wound compromises the dermal layer of the skin.
Stage 3:
Superficial ulcer, primarily on the bony prominence of the nose or any other pressure site clinically visible as an abrasion or a blister. The wound compromised the subcutaneous fat layer of the skin.
Stage 4:
If the pressure exposure continues without any prevention measure or treatment a deep full thickness pressure ulcer will appear. Bone, muscle and tendon may be exposed. The wound bed may be covered by slough.
Table 1 outlines the aforementioned classification system and their associated clinical manifestations.
Prevention Recommendations
Prolonged pressure of PPE to areas of bony prominence with thin overlying skin, such as the orbital rim and nasal bone, is the chief culprit of these facial lesions. Offloading techniques that minimize this pressure on the skin are the most effective means of prevention. Cushioning the infraorbital cheek and nasal bridge help protect the underlying skin from damage. Products such as surgical tape (ie, 3M Microfoam Surgical Tape™) and/or hydrocolloid dressing (ie, DuoDERM™) are effective. Additionally, positioning non-mask PPE, like face shields, in a way that does not put additional pressure on the mask is also beneficial.
It is critical that the seal of the mask is maintained when in use. Some products and application techniques may interfere with this seal, putting the user at risk for infection. If possible, cushioning products should be applied as one continuous strip to help minimize the risk of seal compromise of the mask. If two or more strips of a product are used, they should overlap and be applied firmly in place (Figure 1). A demonstrational video is also available online.9 Application of moisturizer to the face immediately before donning PPE can also interfere with the adherence of tape to the skin and compromise the seal of the mask. Instead, we recommend washing the face with a gentle cleanser prior to applying cushioning products. A seal check should always be done after donning a mask. Additional infor-






