Cytokine Analysis
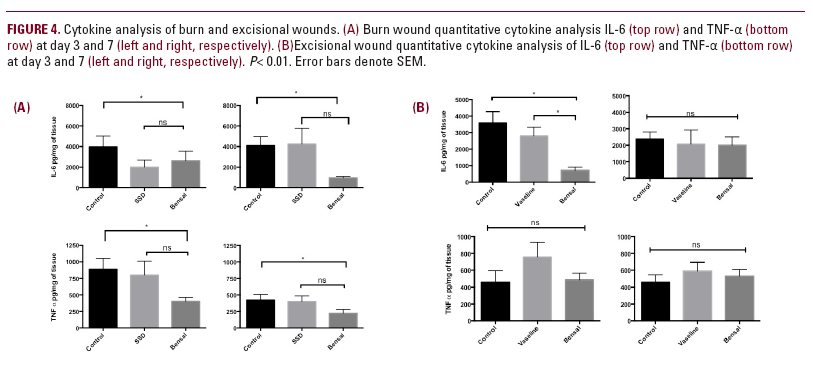
Cytokine analysis (Figure 4a) of burn wounds treated with Bensal
HP showed a significant reduction of both IL-6 and TNFα at days 3 and 7 as compared to untreated controls (2617.0 vs 3966.9 and 954.1 vs 4099.3 pg/mg for IL-6, and 405.1 vs 889.5 and 220.1 vs 426.3 pg/mg for TNFα at days 3 and 7, respectively), with no significant difference when compared to SSD-treated wounds (2617.0 vs 2004.2 and 954.1 vs 4240.2 pg/mg for IL-6, and 405.1 vs 803.2 and 220.1 vs 400.8 pg/mg for TNFα at days 3 and 7, respectively). For excisional wounds (Figure 4b), Bensal HP treatment resulted in a statistically significant decrease in IL-6 expression at day 3 when compared to untreated controls and petrolatum (714.0 vs 3597.0 and 2792.0 pg/mg, respectively). There was no statistical difference appreciated in the expression
of IL-6 at day 7 or TNFα at days 3 and 7.
DISCUSSION
The above results represent the first pre-clinial evaluation of Bensal HP on wound healing. In the setting of burn wounds Bensal HP treatment resulted in limited wound expansion within
the first days post-injury when compared to controls and SSD, though reached closure at the same day as controls. These results were mirrored by histological findings that showed accelerated
maturation of the wound bed by day 17 as compared to other treatment groups, with a statistically significant increase
in collagen deposition in the wound bed in Bensal treated groups. Lastly, both IL-6 and TNFα secretion were decreased in Bensal HP-treated burns when compared to the other groups, though this difference was only statistically significant when compared to controls. In excisional wounds, Bensal HP treatment
resulted in comparable wound healing times as compared to controls and petrolatum. Positive histologic features were seen in both Bensal HP and petrolatum-treated wounds, with both groups exhibiting increased collagen deposition when
compared to controls. Additionally, IL-6 production was significantly
attenuated in the Bensal HP-treated wounds at day 3, with no significant difference seen at day 7. No difference in TNFα expression was appreciated throughout the study interval.
These results are of considerable interest, given the fact that Bensal HP has not been extensively studied as a wound healing adjuvant, even in spite of decades of use. One study by Jacobs et al. found that Bensal HP application to diabetic ulcers resulted in a statistically significant improvement in wound closure when compared to SSD in a human clinical trial.3 Investigators posited that the observed effect could be due to a host of factors including
the antimicrobial efficacy of benzoic acid, and the keratolytic effect of salicylic acid.3 While these results are promising, they are limited and offer no insight into mechanism of action.
Wound healing can be understood in several phases. The first phase post-injury is hemostasis. With the formation of a fibrin clot and platelet aggregation and degranulation, a number of pro-inflammatory cytokines and growth factors are allowed to concentrate in the area of the wound bed. These mediators help to attract various cell types, including neutrophils whose predominance
defines the inflammatory stage of wound healing. Neutrophils help to disinfect the wound and clear damaged tissues through both phagocytosis and the release of proteases
and pro-inflammatory cytokines. It is important to note that these proteases and inflammatory mediators can diffuse into surrounding tissue, allowing wounds (especially burns) to expand within the first few days following injury. Next is the proliferative phase which is characterized by a predominance of macrophages. Macrophages carry out remodeling of the extracellular matrix in concert with fibroblasts. Fibroblasts first lay down a provisional extracellular matrix composed of






