Psoriasis Case Reports
Predicting a Biologic Treatment Fast-Responder Profile in Psoriatic Patients: Advanced Application of Artificial-Neural-Networks (ANNs)
Giovanni Damiani MD, Rosalynn R.Z. Conic MD PhD, Paolo D.M. Pigatto Prof MD, Carlo G. Carrera MD, Chiara Franchi MD, Angelo Cattaneo MD, Piergiorgio Malagoli MD, Radhakrishna Uppala Prof MD PhD, Dennis Linder Prof MD, Nicola L. Bragazzi MD PhD, Enzo Grossi Prof MD
The present study is possibly the first approach employing ANNs to predict drug efficacy in dermatology; a wider use of ANNs may be conducive to useful both theoretical and clinical insight.
Successful Management of a Black Male With Psoriasis and Dyspigmentation Treated With a Novel Combination .01%/.0045% Lotion: Case Report
Seemal R. Desai MD, Andrew F. Alexis MD MPH, Abby Jacobson MS PA-C
Skin of color patients with psoriasis face unique challenges related to disease characteristics and treatment. Dyspigmentation, including postinflammatory hypo- and hyperpigmentation, more frequently and severely affects patients with skin of color and remains a challenge in psoriasis management. We present the case of a 58-year-old Black male with moderate psoriasis who was treated for 8 weeks with a fixed combination novel 0.01%/0.045% lotion during a phase 3 study (NCT02462070).
Topical Cannabinoids for the Management of Psoriasis Vulgaris: Report of a Case and Review of the Literature
Adam J. Friedman MD, Kimia Momeni BS, Mikhail Kogan MD
The interest in use of medical cannabis for chronic dermatologic conditions such as psoriasis, eczema, and acne has been growing mostly owing to rapidly emerging decriminalization across the country and impressive commercially driven popularization of a variety of cannabinoid preparations including topical forms such as creams, salves, lotions, lubricants, and many others. We present a case of a young man with psoriasis managed with topical cannabinoids.
Tumor Necrosis Factor Inhibitor-Induced Psoriasis in a Pediatric Crohn’s Disease Patient Successfully Treated with Another Biologic
Lauren Bonomo , Ellen H. de Moll , Linden Li , Lauren Geller , Michael I. Gordon , David Dunkin
This is the first reported case of a school-age pediatric patient with TNF inhibitor-induced psoriasis treated with another biologic. Controlled trials are warranted to fully assess the safety and efficacy of this biologic for treating TNF inhibitor-induced psoriasis in the pediatric population.
Is TNF-α Inhibitor-Induced Psoriasiform Dermatitis Always Psoriasiform?
Chapman Wei BS, Emily C Murphy MD, Joseph Zahn MD, Adam J. Friedman MD FAAD
Based on the mounting evidence in the literature that TNFI-induced ‘psoriasiform’ eruptions present with a wide spectrum of overlapping morphology and histopathologic features, the characterization of TNFI-induced lesions should rely more on the histopathologic pattern.
Rapid and Sustained Improvement in a Patient With Plaque Psoriasis Switched to Brodalumab After Failing Treatment Clearance on Six Other Biologic Therapies
Psoriasis is a chronic, inflammatory, remitting/relapsing autoimmune condition involving a dysregulated inflammatory response of the interleukin (IL) 23/T-helper (Th)-17 pathway. Greater understanding of the immune-mediated pathology of the disease has led to the development of numerous biological therapies and biosimilars that target the various inflammatory pathways.
Successful Treatment of Refractory Plaque-Type Psoriasis and Psoriatic Arthritis With Novel Biologic Combination Therapy: A Case Report
There is limited data supporting the combination of biological agents in the management of psoriasis and psoriatic arthritis. This is the first case report of plaque psoriasis with arthritis, successfully treated with two biologic combination therapy, without concurrent use of other systemic agents during the treatment. However, further studies need to be carried out to evaluate the efficacy and safety of this biologic combination therapy.
Ostraceous Psoriasis Presenting as Koebner Phenomenon in a Tattoo
Psoriasis is a common dermatologic condition with a variety of morphologic presentations. These variations include the less common hyperkeratotic form, psoriasis ostracea, defined as having pronounced adherent scales resembling an oyster shell. Of the ostraceous cases that have been reported in the literature, many occur as generalized outbreaks in patients with long-standing history of psoriasis. Rarely does this remarkable variant occur as a direct flare from a cutaneous insult. In these situations, when a pre-existing dermatosis appears in response to a traumatic insult to skin, the process is referred to as the Koebner phenomenon.
Psoriasiform Pemphigus Foliaceus in an African American Female: An Important Clinical Manifestation
A 50-year-old African-American woman presented to the dermatology clinic with a pruritic eruption of 3 years’ duration. On clinical examination, the patient had well-demarcated, pink, atrophic plaques and superficial erosions over the inframammary folds and mid-chest. She also had well-demarcated, hyperpigmented, hyperkeratotic scaly plaques over the abdomen, suprapubic region, elbows, knees, and back with sporadic small superficial blisters.
Sponsored
Podcast Episodes
Picking up on Prescribing Patterns for Psoriasis: A Real Deal Assessment
We (and our patients) are fortunate to live during a time when we have many safe and effective options to treat a chronic inflammatory skin disease such as Psoriasis. We are reminded of this, nay inundated, with warm and fuzzy headlines in the lay dermatology press that humblebrag said efficacy. However, how does this translate to the real world, when the perfect, neat lines of clinical trials are blurred by practical issues such as access, patient and practitioner perception, and long term use and efficacy? In a JDD Podcast first, we had not one but two investigators share their work and first steps to evaluate just that.
To Treat or Not To Treat: Systemic Therapy Considerations for Psoriasis in the Setting of Malignancy
I’m a biologic girl in a biologic world…or so I think myself and never say out loud when reviewing therapeutic options for moderate to severe psoriasis. We are so fortunate to have so many wonderful options, however certain clinical scenarios may limit our ability to capitalize on said armament mostly due to limited experience and data. Enter previous malignancy – in most phase 3 studies these patients are weeded out or the history of malignancy must be at least 5 years prior to entry. So what to do? Our colleagues at Tufts Medical Center asked this very question. Tune in to hear what Dr. David Rosmarin, Assistant Professor of Dermatology and Residency Program Director learned from performing a retrospective chart review and how his work and his experience guides his clinical decision making when managing psoriasis. Don’t flake (or is it scale?)….check it out.
What Women Don’t Want … Psoriasis
Ask the Investigator: Shedding Some Light on Phototherapy Protocols for Psoriasis and Tips to Improve Patient Screening and Treatment
In this edition of the JDD Podcast, Dr. Adam Friedman reviews phototherapy protocols and pearls with psoriasis expert Dr. Jashin Wu, Director of Research at Kaiser Permanente based on his study published in the August 2016 Journal of Drugs in Dermatology titled “Comparison of Phototherapy Guidelines for Psoriasis: A Critical Appraisal and Comprehensive Review.” Also tune in to hear how Dr. Wu counsels his psoriasis patients on psoriasis comorbidities and initiates, and manages them with phototherapy, topicals, and systemic immunosuppressants.
Translational Lecture Series
Targeting cAMP Signaling for the Treatment of Inflammatory Diseases of the Skin
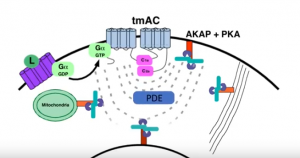 Dr. Jon Zippin elucidates the complexity of cAMP biology and the translational impact of PDE4 inhibition as it relates to chronic inflammatory skin diseases. Tune in to learn why targeting this pathway is clinically meaningful but also where more work is needed to improve outcomes.
Dr. Jon Zippin elucidates the complexity of cAMP biology and the translational impact of PDE4 inhibition as it relates to chronic inflammatory skin diseases. Tune in to learn why targeting this pathway is clinically meaningful but also where more work is needed to improve outcomes.
Psoriasis: Biological Basis for Comorbidities
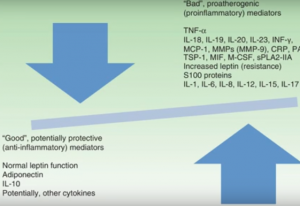 Dr. Abrar Qureshi, Professor and Chair of Department of Dermatology at The Warren Alpert Medical School of Brown University, reviews his research to uncover the biological basis for many of the co-morbidities associated with, and risk factors for, psoriasis. Through this clear and clinically oriented presentation, the common pathophysiological threads are elucidated with a focus on identifying preventive strategies and therapeutic targets for current and future treatments.
Dr. Abrar Qureshi, Professor and Chair of Department of Dermatology at The Warren Alpert Medical School of Brown University, reviews his research to uncover the biological basis for many of the co-morbidities associated with, and risk factors for, psoriasis. Through this clear and clinically oriented presentation, the common pathophysiological threads are elucidated with a focus on identifying preventive strategies and therapeutic targets for current and future treatments.






