Psoriasis
An Unusual Case of Psoriasiform Dermatitis Treated With Dual Biologic Therapy and Literature Review
Previously believed to be of distinct immunopathogenesis, atopic dermatitis (AD) and psoriasis (PsO) spectrum may permit immunologic shifts to favor the opposing inflammatory states following biologic treatment. Cases of AD that developed following PsO biologics are increasingly reported in the literature.
A Review of the Safety and Efficacy of Deucravacitinib for Plaque Psoriasis: An Expert Consensus Panel
Psoriasis is a chronic, inflammatory disease associated with numerous negative physical and psychosocial impacts. Deucravacitinib is a novel, selective TYK2 inhibitor approved by the FDA for the treatment of moderate-to-severe plaque psoriasis in adults.
Structural Insights: What Makes Some IL-23 Biologics More Effective in Psoriasis
Psoriasis is a chronic inflammatory skin disease affecting over 7.5 million adults in the United States, and over 41 million people worldwide.
The Hidden Costs of Psoriasis: A Population-Based Study Evaluating How Psoriasis Severity Impacts Work Absenteeism
Psoriasis patients experience physical and emotional burdens, which may lead to work-related productivity loss. This loss carries professional and financial repercussions. It is unknown whether the extent of psoriasis affects work absenteeism.
Real-Life Effectiveness and Safety of Guselkumab in Moderate-to-Severe Plaque Psoriasis: A 104-Week Retrospective Single-Center Study
Guselkumab is a monoclonal antibody approved for treating moderate-to-severe plaque psoriasis. Long-term data on the effectiveness and safety of guselkumab in a real-world setting are still limited.
First Use of Combination Oral Deucravacitinib With Tapinarof Cream for Treatment of Severe Plaque Psoriasis
Plaque psoriasis is a chronic, immune-mediated, cutaneous, and systemic inflammatory dermatosis. Its pathogenesis involves the dysregulation of the interleukin (IL)-23/IL-17 signaling pathway.
The Patient-Physician Relationship and Adherence: Observations From a Clinical Study
Improved patient-physician relationships (PPR) are associated with better patient satisfaction and disease outcomes, however, there is limited literature assessing how PPR affects adherence in dermato…
Antimalarials are not Effective as Pre-Exposure Prophylaxis for COVID-19: A Retrospective Matched Control Study
The early phase of the COVID-19 pandemic prompted a repurposing of antiviral and immunomodulatory drugs as investigational therapeutics, including hydroxychloroquine and chloroquine. While antimalaria…
Biologic Vs Conventional Therapies: Comparing Risk of Psoriasis-Associated Comorbidities
Psoriasis is associated with multiple comorbidities. In this retrospective cohort analysis, we compared the comorbidities in patients who received biologic treatments with those who received conventional treatments. Our data indicates that biologics may be associated with lower rates of comorbidities in comparison to conventional therapy.
Cross-Sectional Study of Psoriasis, Atopic Dermatitis, Rosacea, and Alopecia Areata Suggests Association With Cardiovascular Diseases
Background: A growing body of evidence suggests that several inflammatory skin diseases (ISDs) are associated with systemic inflammation and cardiovascular disease (CVDs).
Evaluating Sentiment, Engagement, and Perception of Biologics Among Patients
With Psoriasis and Psoriatic Arthritis on Reddit
Background: Limited analyses of social media content among psoriasis (PsO) and psoriatic arthritis (PsA) patients exist. These patients may turn to social media to gain insight into treatments such as biologics.
Patient Preference for Calcipotriene and Betamethasone Dipropionate Cream
Versus Foam for the Topical Treatment of Psoriasis: A Pilot Study
Background: The well-established sequential use of topical calcipotriene and topical betamethasone dipropionate in combination has been shown to provide greater benefit than either monotherapy…
Breaking the Frustrating Cycle of Topical Steroids in Psoriasis: A Review of a Novel Vehicle for Fixed-Dose Combination Halobetasol Propionate/Tazarotene
Topical therapies are commonly used to treat psoriasis, either as monotherapy for milder disease or as adjuncts to systemic and biologic drugs. Topical steroids and tazarotene are both options for topical psoriasis treatment, but as monotherapies, they are associated with adverse events (AEs) that make adherence to prescribed treatment challenging.
An Investigator-Initiated Trial of a Polymeric Emulsion of Halobetasol Propionate and Tazarotene in the Treatment of Palmoplantar Psoriasis
Objective: To evaluate the synergistic effect of a fixed-combination topical lotion composed of halobetasol propionate 0.01% and tazarotene 0.045% in the treatment of palmoplantar psoriasis.
Efficacy and Safety of Water-Free Lipid Formulation System Containing Calcipotriol Against Psoriasis Vulgaris
Calcipotriol, a vitamin D analogue is widely used in the treatment of psoriasis. However, poor adherence to topical therapy has led to an ineffective use of the medication and built a barrier to the treatment’s success. A water-free lipid-based formulation system has been developed to improve dosage and cosmetic properties along with patient compliance…
Meeting Patient Expectations of Topical Psoriasis Treatment: Evidence Supporting the Use of Fixed-Combination Halobetasol/Tazarotene Lotion
Discordance between patient and clinician treatment goals and expectations can present a challenge to implementation of effective therapeutic plans. Because topical treatments are commonly used for plaque psoriasis, both as monotherapy and adjuncts to other treatment modalities, providers need to understand the concerns of patients with psoriasis regarding use of topical products…
Examining the Potential for Koebnerization and Disease Precipitation in Cicatricial Alopecias
The treatment of primary scarring alopecias is challenging and patients may be susceptible to koebnerization. This predisposes cicatricial alopecia patients to worsening of their disease following procedural treatments or interventions.
Unmet Needs in Psoriasis Patients
Psoriasis can greatly impact patients’ quality of life. The introduction of new treatments has improved treatment outcomes, but treatment gaps may still exist. Participants aged 18 years or older, with an Amazon Mechanical Turk account, who reported diagnosis of psoriasis and correctly answered an attention check question were included. Results were analyzed using descriptive and inferential statistics.
Persistence With Biologic Treatments in Psoriasis: A Structured Literature Review of Studies Using Administrative Database and Clinical Registry Data
Psoriasis is a chronic, autoimmune-mediated inflammatory disorder. Persistence rates calculated from these two data sources appear to be systematically different.
New Biologics and Oral Drugs in Treatment of Moderate to Severe Psoriasis
Psoriasis is known to have no definitive cure, which is in common with other inflammatory disorders. Various treatment options are available, and they help in decreasing the disease activity and improving symptoms.
Treatment of Scalp Psoriasis
Scalp involvement is seen in a majority of individuals with psoriasis, a chronic autoimmune skin disease with variable phenotypes.
Increased Trend of Cosmetic Procedures in Patients With Psoriasis Who Attain 75% or Greater Improvement
Is there a relationship between the clearance of psoriasis, improved quality of life and cosmetic procedures?
Case Reports
Severe Psoriasis Presenting in 3-Year-Old Child With Nail Dystrophy: Response to Biologic Treatment
Psoriasis, a chronic inflammatory skin condition, affects about 2% of children. A small subset have isolated nail involvement refractory to topical treatment that can be disabling.
Successful Treatment of Refractory Plaque-Type Psoriasis and Psoriatic Arthritis: A Case Report
A unique case of severe plaque psoriasis, psoriatic arthritis and successful treatment with unique biologic combination after failure of prior topical and narrow-band ultraviolet B (NBUVB) phototherapy.
Supplements
Do You Know the Most Complete, Targeted Biologic for Psoriasis? The Answer May Surprise You
Early in the 1980s, topical therapy was the mainstay for medical management of this skin condition. Three decades later, dermatologists have a much better understanding of the pathogenesis of psoriasis and its related comorbidities. Novel therapies have emerged to target the immunologic drivers at the heart of the disease.
IL-23 Versus IL-17 in the Pathogenesis of Psoriasis: There Is More to the Story Than IL-17A
Explore the importance of the TH17 pathway in psoriasis pathogenesis with a focus on the roles of IL-23 and IL-17 within this pathway. Discuss the different IL-17 subtypes involved in psoriasis immunopathology and the multitude of cells that can produce these subtypes. Examine treatments that inhibit IL-23 and IL-17.
Podcast Episodes
What Women Don’t Want … Psoriasis
Picking up on Prescribing Patterns for Psoriasis: A Real Deal Assessment
We (and our patients) are fortunate to live during a time when we have many safe and effective options to treat a chronic inflammatory skin disease such as Psoriasis. We are reminded of this, nay inundated, with warm and fuzzy headlines in the lay dermatology press that humblebrag said efficacy. However, how does this translate to the real world, when the perfect, neat lines of clinical trials are blurred by practical issues such as access, patient and practitioner perception, and long term use and efficacy? In a JDD Podcast first, we had not one but two investigators share their work and first steps to evaluate just that.
To Treat or Not To Treat: Systemic Therapy Considerations for Psoriasis in the Setting of Malignancy
I’m a biologic girl in a biologic world…or so I think myself and never say out loud when reviewing therapeutic options for moderate to severe psoriasis. We are so fortunate to have so many wonderful options, however certain clinical scenarios may limit our ability to capitalize on said armament mostly due to limited experience and data. Enter previous malignancy – in most phase 3 studies these patients are weeded out or the history of malignancy must be at least 5 years prior to entry. So what to do? Our colleagues at Tufts Medical Center asked this very question. Tune in to hear what Dr. David Rosmarin, Assistant Professor of Dermatology and Residency Program Director learned from performing a retrospective chart review and how his work and his experience guides his clinical decision making when managing psoriasis. Don’t flake (or is it scale?)….check it out.
Light It Up Up Up: Phototherapy Is Still a Big Fish In The Sea of Therapeutic Options for Psoriasis
Let’s face it, we are faced (redundancy…on purpose) with almost too many therapeutic options for the management of plaque Psoriasis. Absolutely a good problem to have, even better for our patients, but it can also be the source of a management riddle: Erythema isn’t always red, Nevi can be blue, with all of these systemic agents, should you be using phototherapy too? Yes, simply yes. Tune in as JDD Podcast host Dr. Adam Friedman gets to these burning questions with renaissance dermatologist Dr. Peter Lio. With all the great practical information highLIGHTed, this podcast will certainly brighten your day.
Ask the Investigator: Shedding Some Light on Phototherapy Protocols for Psoriasis and Tips to Improve Patient Screening and Treatment
In this edition of the JDD Podcast, Dr. Adam Friedman reviews phototherapy protocols and pearls with psoriasis expert Dr. Jashin Wu, Director of Research at Kaiser Permanente based on his study published in the August 2016 Journal of Drugs in Dermatology titled “Comparison of Phototherapy Guidelines for Psoriasis: A Critical Appraisal and Comprehensive Review.” Also tune in to hear how Dr. Wu counsels his psoriasis patients on psoriasis comorbidities and initiates, and manages them with phototherapy, topicals, and systemic immunosuppressants.
Video Pearls
In a compelling video interview for the Journal of Drugs in Dermatology, Dr. Christopher Bunick delves into the evolving landscape of moderate-to-severe plaque psoriasis, with a special emphasis on the IMMPulse Head-to-Head Study. As a leading expert in dermatologic therapeutics, he shares how molecular insights into PDE4 inhibition set the stage for a rigorous comparison of apremilast and the IL-23 inhibitor risankizumab.
Psoriasis: Biological Basis for Comorbidities
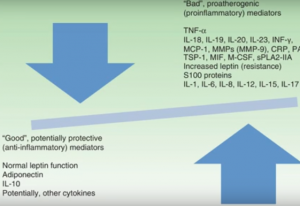 Dr. Abrar Qureshi, Professor and Chair of Department of Dermatology at The Warren Alpert Medical School of Brown University, reviews his research to uncover the biological basis for many of the co-morbidities associated with, and risk factors for, psoriasis. Through this clear and clinically oriented presentation, the common pathophysiological threads are elucidated with a focus on identifying preventive strategies and therapeutic targets for current and future treatments.
Dr. Abrar Qureshi, Professor and Chair of Department of Dermatology at The Warren Alpert Medical School of Brown University, reviews his research to uncover the biological basis for many of the co-morbidities associated with, and risk factors for, psoriasis. Through this clear and clinically oriented presentation, the common pathophysiological threads are elucidated with a focus on identifying preventive strategies and therapeutic targets for current and future treatments.
Translational Lecture Series
Targeting cAMP Signaling for the Treatment of Inflammatory Diseases of the Skin
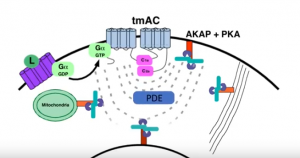 Dr. Jon Zippin, elucidates the complexity of cAMP biology and the translational impact of PDE4 inhibition as it relates to chronic inflammatory skin diseases. Learn why targeting this pathway is clinically meaningful and where more work is needed to improve outcomes.
Dr. Jon Zippin, elucidates the complexity of cAMP biology and the translational impact of PDE4 inhibition as it relates to chronic inflammatory skin diseases. Learn why targeting this pathway is clinically meaningful and where more work is needed to improve outcomes.
Psoriasis: Biological Basis for Comorbidities
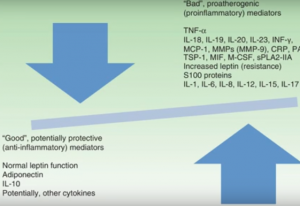 Dr. Abrar Qureshi, Professor and Chair of Department of Dermatology at The Warren Alpert Medical School of Brown University, reviews his research to uncover the biological basis for many of the co-morbidities associated with, and risk factors for, psoriasis. Through this clear and clinically oriented presentation, the common pathophysiological threads are elucidated with a focus on identifying preventive strategies and therapeutic targets for current and future treatments.
Dr. Abrar Qureshi, Professor and Chair of Department of Dermatology at The Warren Alpert Medical School of Brown University, reviews his research to uncover the biological basis for many of the co-morbidities associated with, and risk factors for, psoriasis. Through this clear and clinically oriented presentation, the common pathophysiological threads are elucidated with a focus on identifying preventive strategies and therapeutic targets for current and future treatments.







