The JDD is committed to publishing the latest public health research, updates, and information to help providers better serve patients. Discover global health manuscripts, supplements, podcast episodes, and more below.
The JDD is committed to publishing the latest public health research, updates, and information to help providers better serve patients. Discover global health manuscripts, supplements, podcast episodes, and more below.

Far far away, behind the word mountains, far from the countries Vokalia and Consonantia, they live.
Natural and manmade disasters cause a range of dermatologic manifestations, including secondary infections after a flood,1 irritation from blistering agents used in chemical warfare,2 or acute and chronic effects of cutaneous radiation syndrome.3
Although oxygen is essential for proper wound healing, wounds are often hypoxic with diminished oxygen delivery to the healing tissue. Since oxygenation of the outer layers of skin is almost exclusively provided by the atmosphere, increasing the presence of external oxygen enhances the healing process. Hyperbaric oxygen therapy is beneficial for treating nonhealing wounds, such as diabetic ulcers, and has been used to speed post-treatment recovery following aesthetic procedures; however, it is not suitable for home use. Recently, perfluorocarbon emulsions have been developed that can absorb large amount of oxygen. Preparations containing 2% of these compounds can absorb up to seven-times more oxygen than water at 37°C. A topical perfluorocarbon emulsion consisting of perfluorodecalin, water, plant derived emulsifiers, and a preservative, has been developed for use in dermatology (Cutagenix™ & Cutavive™ Professional Skin Care Emulsion; Cutagenesis, Niwot, CO). Designed to be applied 2 to 4 times daily following skin rejuvenation procedures, this topical oxygen emulsion reduces the incidence of post-procedure complications. The application of a topical emulsion is well-suited for patient application to enhance recovery following energy-based aesthetic procedures.
A large proportion of data on photoprotective practices is yielded from free skin cancer screenings. However, the sun safety practices of populations who seek these skin cancer screenings may differ from the general public. To examine differences in skin cancer prevention practices and risk factors, we surveyed pedestrians at six locations in Washington, DC (public group, n=285) and attendees of a free skin cancer screening (screening group, n=144) using an IRB-approved survey. The screening group was older and included more individuals with fair skin than the public group. Respondents from the screening group were significantly more likely to always wear sunscreen, always seeks shade, and always or sometimes wear sun-protective clothing than the public group (P<0.05). To examine whether younger and non-white participants, who were less likely to attend our free screening, have different practices and risk factors than older and white participants, respectively, we compared survey answers for all participants by age and race. White participants were more likely to always or sometimes wear sunscreen and sun-protective clothing than non-white participants (P<0.05). Patients over 61 years were more likely to always seek shade and wear sun-protective clothing than those younger than 31 years (P<0.05). Therefore, free skin cancer screenings need to be better popularized among non-white and younger populations or more effective educational vehicles are needed.
BACKGROUND: Recent research has identified potential uses of cannabinoids in dermatology, including psoriasis, atopic dermatitis, and wound healing. OBJECTIVE: The extent of dermatologists’ familiarity with and interest in cannabinoids as therapeutics is unknown. METHODS: This study examined dermatology providers’ knowledge, attitudes, and perceptions on therapeutic cannabinoids using a 20-question online survey. RESULTS: The response rate was 21% (n=531). Most responders thought cannabinoids should be legal for medical treatment (86%). Nearly all (94%) believed it is worthwhile to research dermatologic uses of cannabinoids. 55% reported at least one patient-initiated discussion about cannabinoids in the last year. Yet, 48% were concerned about a negative stigma when proposing cannabinoid therapies to patients. While most responders (86%) were willing to prescribe an FDA-approved cannabinoid as a topical treatment, fewer (71%) were willing to prescribe an oral form. 64% of respondents did not know that cannabidiol is not psychoactive and 29% did not know that tetrahydrocannabinol is psychoactive. LIMITATIONS: Limited survey population. CONCLUSIONS: Dermatology providers are interested in prescribing cannabinoids and patients are speaking about cannabinoids with their dermatologists. However, providers’ fund of knowledge on this subject is lacking. These results highlight the need for further education and research to detangle the dermatologic benefits and risks of cannabinoids. J Drugs Dermatol. 2018;17(12):1273-1278.
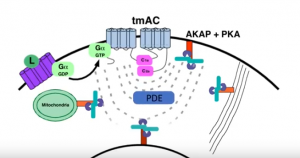 Dr. Jon Zippin, Assistant Attending Dermatologist and Assistant Professor of Dermatology at Weill Medical College of Cornell, elucidates the complexity of cAMP biology and the translational impact of PDE4 inhibition as it relates to chronic inflammatory skin diseases. Tune in to learn why targeting this pathway is clinically meaningful but also where more work is needed to improve outcomes.
Dr. Jon Zippin, Assistant Attending Dermatologist and Assistant Professor of Dermatology at Weill Medical College of Cornell, elucidates the complexity of cAMP biology and the translational impact of PDE4 inhibition as it relates to chronic inflammatory skin diseases. Tune in to learn why targeting this pathway is clinically meaningful but also where more work is needed to improve outcomes.
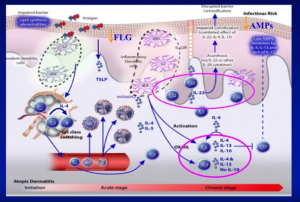 Dr. Amy Paller, Walter J. Hamlin Professor and Chair of Dermatology & Professor of Pediatrics at Northwestern University Feinberg School of Medicine in Chicago, Illinois, delivers a presentation discussing the cause and treatment of pediatric Atopic Dematitis, including co-morbidities, epidermal barrier impairment, and compliance issues.
Dr. Amy Paller, Walter J. Hamlin Professor and Chair of Dermatology & Professor of Pediatrics at Northwestern University Feinberg School of Medicine in Chicago, Illinois, delivers a presentation discussing the cause and treatment of pediatric Atopic Dematitis, including co-morbidities, epidermal barrier impairment, and compliance issues.
 Dr. Gil Yosipovitch, Professor of Dermatology at University of Miami Miller School of Medicine, provides residents and physicians access to the latest bench research and practical pearls from a master in pruritus that will help them offer the highest quality evidence-based dermatological care.
Dr. Gil Yosipovitch, Professor of Dermatology at University of Miami Miller School of Medicine, provides residents and physicians access to the latest bench research and practical pearls from a master in pruritus that will help them offer the highest quality evidence-based dermatological care.