INTRODUCTION
Dissecting cellulitis of the scalp (DCS) is a chronic inflammatory disorder of the scalp that manifests as inflamed nodules and abscesses, with subsequent patchy, scarring hair loss.1 While its exact pathogenesis remains unclear, follicular occlusion, inflammation, and sinus tract formation are thought to be key contributors.1 DCS is commonly associated with hidradenitis suppurativa (HS), acne conglobata (AC), and pilonidal cysts, collectively known as the follicular occlusion tetrad.1 The condition can be significantly debilitating due to pain, visual disfigurement, and psychological distress.1 We present two patients with refractory DCS and concomitant HS and AC who were successfully treated with a combination therapy regimen of bimekizumab, isotretinoin, and oral antibiotics.
CASE REPORTS
A 26-year-old male with a medical history significant for HS and AC presented to our dermatology clinic with a greater than 10-year history of draining sores on his scalp and associated hair loss (Figure 1). At the time of presentation, the patient had already been diagnosed with biopsy-proven DCS from an outside dermatologist. Previously trialed and failed treatments included adalimumab, isotretinoin, oral tetracycline, doxycycline, minocycline, and incision and drainage of the nodules. On physical examination, he had multiple scarring alopecic patches with surrounding erythematous pustules and nodules on the scalp, face, and chest. Although his medical history was also significant for nodules and abscesses within the inguinal folds and chest, they were not observed on exam. The patient was
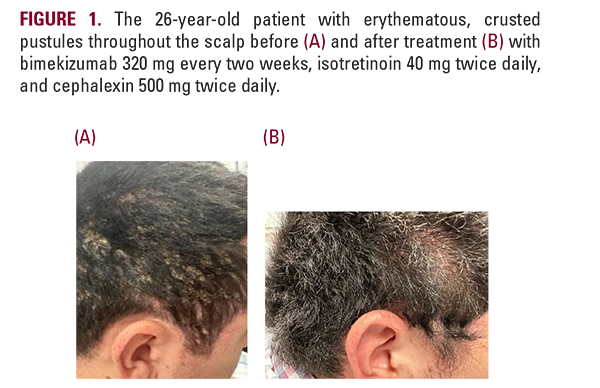
subsequently started on bimekizumab 320 mg, cephalexin 500 mg twice daily, and isotretinoin 40 mg twice daily. At the initial visit, the patient received a loading dose of bimekizumab 320 mg and then switched to bimekizumab 160 mg every two weeks. After 6 weeks following the initial loading dose, the patient achieved complete resolution of scalp lesions (Figure 1). The patient is continuing the bimekizumab 160 mg maintenance dosing, cephalexin 500 mg twice daily, and isotretinoin 40 mg twice daily to maintain clearance of his condition.
A 33-year-old patient from Australia presented with a 4-year history of HS, AC, and DCS, primarily concerned about the increasing number of nodules developing on his scalp and scattered areas of hair loss. He had previously tried and failed
A 33-year-old patient from Australia presented with a 4-year history of HS, AC, and DCS, primarily concerned about the increasing number of nodules developing on his scalp and scattered areas of hair loss. He had previously tried and failed






