INTRODUCTION
Granuloma annulare (GA) is a granulomatous inflammatory skin condition of unknown etiology, often presenting as annular plaques or papules.1 Generalized GA (GGA) is a rare subtype of GA characterized by its widespread distribution and resistance to conventional treatments such as topical or intralesional corticosteroids.2 The rarity of the disease and lack of evidence-based treatment guidelines pose a unique management challenge. Biologics and oral JAK inhibitors have increasingly been used for refractory GGA cases.3 We sought to characterize the outcomes of these therapies used for GGA in a large academic center.
GA is characterized by an upregulation of Th1, Th2, Th17, Th22, and JAK-STAT pathways. There is an increased expression of cytokines such as TNF-α, IL-1β, IFN-γ, IL-12/23p40, IL-4, and IL-31.2 Due to the upregulation of these inflammatory pathways in GA, therapies that target these pathways have been used off-label to treat GGA.4 Several reports have shown improvement or remission with systemic therapies, including JAK inhibitors, TNF-ɑ inhibitors, IL-4 blockers, and IL-23 blockers.4
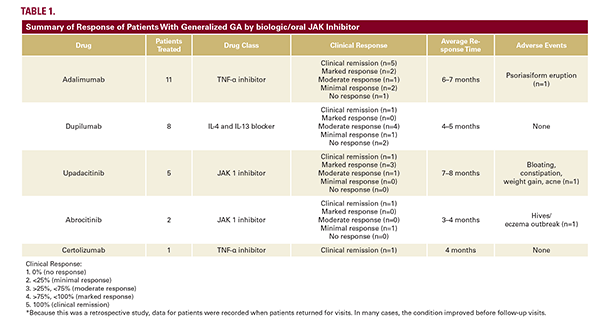
We conducted a retrospective case series of adult GGA patients treated with a biologic or oral JAK inhibitor at a single academic dermatology clinic (November 2016 to January 2025). Patient demographics, medical history, disease extent, and treatment response, assessed by changes in erythema, induration, and lesion count were obtained via medical records (Table 1).
GA is characterized by an upregulation of Th1, Th2, Th17, Th22, and JAK-STAT pathways. There is an increased expression of cytokines such as TNF-α, IL-1β, IFN-γ, IL-12/23p40, IL-4, and IL-31.2 Due to the upregulation of these inflammatory pathways in GA, therapies that target these pathways have been used off-label to treat GGA.4 Several reports have shown improvement or remission with systemic therapies, including JAK inhibitors, TNF-ɑ inhibitors, IL-4 blockers, and IL-23 blockers.4
We conducted a retrospective case series of adult GGA patients treated with a biologic or oral JAK inhibitor at a single academic dermatology clinic (November 2016 to January 2025). Patient demographics, medical history, disease extent, and treatment response, assessed by changes in erythema, induration, and lesion count were obtained via medical records (Table 1).
CASE SERIES
We identified 22 patients (mean age 59.4 years; range 32–77), 90% (n=20) females, and 77% white (Table 2). All patients had recalcitrant disease, having previously attempted corticosteroids (topical, intralesional, or oral), topical ruxolitinib (n=4), hydroxychloroquine (n=6), oral antibiotics (n=6), and phototherapy (n=3).
Adalimumab was the most prescribed therapy (n=11), 63.6% experienced marked response or remission. Dupilumab (n=8) led to moderate or better responses in 62.5% of patients, and one achieved remission. All patients on upadacitinib (n=5) had a positive response, with 80% noting a marked response or remission. Among the 2 patients on abrocitinib, one achieved
Adalimumab was the most prescribed therapy (n=11), 63.6% experienced marked response or remission. Dupilumab (n=8) led to moderate or better responses in 62.5% of patients, and one achieved remission. All patients on upadacitinib (n=5) had a positive response, with 80% noting a marked response or remission. Among the 2 patients on abrocitinib, one achieved