INTRODUCTION
Lichen simplex chronicus (LSC) is a debilitating chronic itch condition, affecting up to 12% of the population, severely impacting patients' quality of life. It is characterized by lichenified skin secondary to intractable itch. Frequent scratching is an impetus for skin barrier disruption, leading to a pro-inflammatory state, sensory dysfunction, and an activated itch-scratch cycle, further perpetuating the condition. The pathogenesis of LSC is unclear. It is thought to be a non-histaminergic process mediated by pruritogen binding to G-protein coupled receptors or ion channels, particularly transient receptor potential channels, which may be an essential component in interleukin 31 (IL-31)-mediated itch.1 Lichen simplex chronicus remains challenging to treat, with current options including topical calcineurin inhibitors, topical steroids, gabapentinoids, antidepressants, and dupilumab.1 Here, we report the resolution of lichen simplex chronicus, previously refractory to a multitude of treatments, with nemolizumab.
Report of a Case
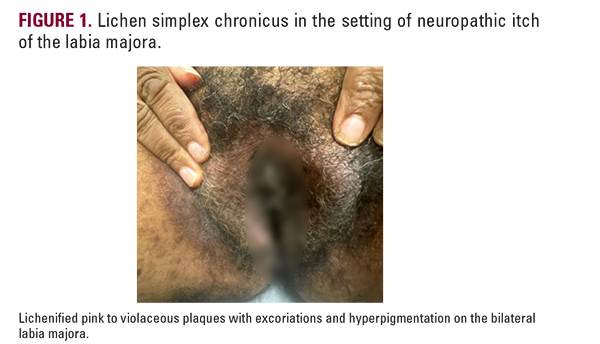
A 52-year-old woman presented with an 8-year history of pruritus of the labia majora, which she described as burning and localized. The patient had a past medical history of hyperlipidemia, polycystic ovarian syndrome, prediabetes, atopic dermatitis, and, notably, an L4-L5 disc bulge secondary to a car accident 9 years prior. The patient had difficulty at work due to the constant itch she was experiencing, as well as her poor sleep. The pruritus was refractory to intralesional triamcinolone injections, a compounded ketamine, amitriptyline, and lidocaine (KAL) formulation, silver sulfadiazine cream, and pramoxine hydrochloride lotion. She did not tolerate gabapentin or pregabalin. Clobetasol and halobetasol did provide symptom relief but were discontinued due to the risk of atrophy from chronic use. The patient's physical exam is shown in Figure 1.
She was diagnosed with LSC in the setting of neuropathic pruritus secondary to bulging L4-5 discs. She was started on nemolizumab, which provided the patient with immediate relief. She received an initial loading dose of 60 mg injected subcutaneously, followed by 30 mg injections every 4 weeks. Just prior to receiving nemolizumab, the patient described the
Report of a Case
A 52-year-old woman presented with an 8-year history of pruritus of the labia majora, which she described as burning and localized. The patient had a past medical history of hyperlipidemia, polycystic ovarian syndrome, prediabetes, atopic dermatitis, and, notably, an L4-L5 disc bulge secondary to a car accident 9 years prior. The patient had difficulty at work due to the constant itch she was experiencing, as well as her poor sleep. The pruritus was refractory to intralesional triamcinolone injections, a compounded ketamine, amitriptyline, and lidocaine (KAL) formulation, silver sulfadiazine cream, and pramoxine hydrochloride lotion. She did not tolerate gabapentin or pregabalin. Clobetasol and halobetasol did provide symptom relief but were discontinued due to the risk of atrophy from chronic use. The patient's physical exam is shown in Figure 1.
She was diagnosed with LSC in the setting of neuropathic pruritus secondary to bulging L4-5 discs. She was started on nemolizumab, which provided the patient with immediate relief. She received an initial loading dose of 60 mg injected subcutaneously, followed by 30 mg injections every 4 weeks. Just prior to receiving nemolizumab, the patient described the