Letter to the Editor:
Administrative burdens, particularly prior authorization (PA) requirements and appeals, remain a significant barrier to timely dermatologic care. On average, physicians complete 39 PAs per week, dedicating 13 hours of staff and clinician time.1 Nationally, 93% of physicians report that PAs delay access to necessary treatment, with one study reporting a median delay of 12 days to initiate care.1,2 As a result, patients frequently arrive to clinic without having started any treatment due to the inability to obtain prescribed medications. In a 2024 national survey, 82% of physicians noted that PA can lead to treatment abandonment and 89% indicated that PAs contribute to burnout.1 These data underscore the urgency of addressing administrative inefficiencies in dermatology. In response, we implemented a quality improvement initiative to increase provider awareness and use of compounded medications as alternatives when standard therapies were denied.
Dermatology residents and attending physicians at an academic medical center participated in targeted educational sessions covering the risks and benefits of compounded medications, appropriate clinical indications, ordering procedures, and patient counseling. Physicians were encouraged to offer compounded alternatives when a PA for a prescribed medication was denied in lieu of proceeding to an appeal.
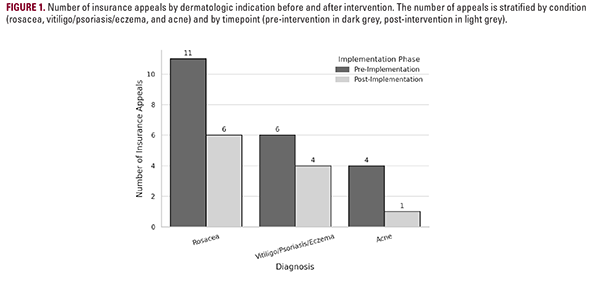
To evaluate the intervention's impact, we compared the frequency of appeals three months before and after training using a chi-square test. The distribution of public vs private insurance did not differ significantly between groups. Following implementation, the proportion of appeals decreased from 6.7% to 2.5% (P=0.0081), suggesting that increased provider familiarity with compounding options may reduce administrative workload without compromising care (Figure 1). Informal feedback also indicated greater provider confidence in navigating compounded alternatives.
This initiative represents a scalable strategy to improve access to dermatologic treatment and reduce administrative burden. Incorporating compounding education into dermatology training may enhance efficiency and promote patient-centered care, particularly when insurance barriers preclude timely
Administrative burdens, particularly prior authorization (PA) requirements and appeals, remain a significant barrier to timely dermatologic care. On average, physicians complete 39 PAs per week, dedicating 13 hours of staff and clinician time.1 Nationally, 93% of physicians report that PAs delay access to necessary treatment, with one study reporting a median delay of 12 days to initiate care.1,2 As a result, patients frequently arrive to clinic without having started any treatment due to the inability to obtain prescribed medications. In a 2024 national survey, 82% of physicians noted that PA can lead to treatment abandonment and 89% indicated that PAs contribute to burnout.1 These data underscore the urgency of addressing administrative inefficiencies in dermatology. In response, we implemented a quality improvement initiative to increase provider awareness and use of compounded medications as alternatives when standard therapies were denied.
Dermatology residents and attending physicians at an academic medical center participated in targeted educational sessions covering the risks and benefits of compounded medications, appropriate clinical indications, ordering procedures, and patient counseling. Physicians were encouraged to offer compounded alternatives when a PA for a prescribed medication was denied in lieu of proceeding to an appeal.
To evaluate the intervention's impact, we compared the frequency of appeals three months before and after training using a chi-square test. The distribution of public vs private insurance did not differ significantly between groups. Following implementation, the proportion of appeals decreased from 6.7% to 2.5% (P=0.0081), suggesting that increased provider familiarity with compounding options may reduce administrative workload without compromising care (Figure 1). Informal feedback also indicated greater provider confidence in navigating compounded alternatives.
This initiative represents a scalable strategy to improve access to dermatologic treatment and reduce administrative burden. Incorporating compounding education into dermatology training may enhance efficiency and promote patient-centered care, particularly when insurance barriers preclude timely