INTRODUCTION
Benign Familial Pemphigus (Hailey-Hailey Disease [HHD]) is caused by a mutation within ATP2C1, the gene encoding the calcium pump of golgi apparatuses, impacting keratinocytes' ability to adhere to each other, resulting in acantholysis.1 Clinical presentation of HHD encompasses blisters that become erythematous plaques and fissures within flexural areas on a relapsing basis. There is no current cure for HHD, so treatments focus on therapeutic management of disease flares and symptoms. Common approaches include topical corticosteroids and antimicrobials for superimposed infections. The authors present a case of ruxolitinib cream, a Janus kinase (JAK) inhibitor, used as a novel treatment for HHD.
CASE REPORT
A 72-year-old female presented to the clinic for evaluation and management of previously diagnosed HHD. Symptoms began in her twenties with pruritic plaques, followed by blisters in the inframammary region, axilla, waist, and inguinal creases that would crust over and develop post-inflammatory hyperpigmentation. Pruritus would last approximately 1 to 2 weeks and resolve after approximately 1 month. In her mid-30s, a dermatologist treated her with Grenz ray, emitting radiation shown to reduce Langerhans cells. The Grenz ray was used intermittently for several decades until it lost efficacy. Since then, she has had numerous episodes that have incapacitated her, reporting a severe lack of self-confidence that prohibited her from attending social engagements and made leaving the house increasingly difficult.
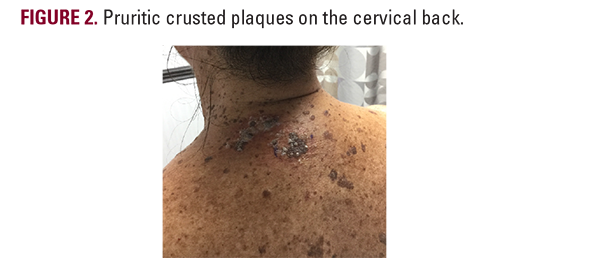
Subsequently, she was prescribed hydrocortisone and antibiotics, which were unsuccessful. Upon visiting the clinic, she endorsed regular flares on her inframammary region (Figure 1), interscapular back (Figure 2), neck, and chest (Figure 3,4). Treatment began with clobetasol ointment twice a day as needed (BID PRN), which proved to be minimally effective.
Subsequently, she was prescribed hydrocortisone and antibiotics, which were unsuccessful. Upon visiting the clinic, she endorsed regular flares on her inframammary region (Figure 1), interscapular back (Figure 2), neck, and chest (Figure 3,4). Treatment began with clobetasol ointment twice a day as needed (BID PRN), which proved to be minimally effective.