ARTICLE: Clinical Insights About the Role of pH in Atopic Dermatitis
December 2019 | Volume 18 | Issue 12 | Supplement Individual Articles | 215 | Copyright © December 2019
Charles Lynde MD FRCPC
American Board of Dermatology, Royal College of Physicians and Surgeons of Canada, Department of Medicine, University of Toronto, Toronto, ON, Canada, Lynderm Research, Markham, ON, Canada
Jerry Tan MD FRCPC
Royal College of Physicians and Surgeons of Canada, Schulich School of Medicine and Dentistry, Department of Medicine, Western University, Windsor, ON, Canada, Windsor Clinical Research Inc., The Healthy Image Centre, Windsor, ON, Canada Sandra Skotnicki MD FRCPC
American Board of Dermatology, the Royal College of Physicians and Surgeons of Canada, Department of Medicine, Divisions of Dermatology, and Occupational and Environmental Health, University of Toronto, Toronto, ON, Canada, Bay Dermatology Centre, Toronto, ON, Canada Anneke Andriessen PhD
Radboud UMC, Nijmegen and Andriessen Consultants, Malden, The Netherlands
Jennifer Beecker MD CCFP(EM) FRCPC DABD
Royal College of Physicians and Surgeons of Canada, American Board of Dermatology, University of Ottawa, Ottawa, ON, Canada, The Ottawa Hospital, Director of Research, The Ottawa Hospital Research Institute, Ottawa, ON, Canada
Joël Claveau MD FRCPC
American Board of Dermatology, Royal College of Physicians and Surgeons of Canada, Department of Medicine, Laval University, Quebec City, QC, Canada; Melanoma and Skin Clinic, Le Centre Hospitalier Universitaire de Québec, Hôtel-Dieu de Québec, Quebec City, QC, Canada
Monica K. Li MD FRCPC
Royal College of Physicians and Surgeons of Canada, Faculty of Medicine, Department of Dermatology and Skin Science, University of British Columbia, Vancouver, BC, Canada, Enverus Medical, Surrey, BC, Canada and Cosmetic Dermatologist, City Medical Aesthetics Center, Vancouver, BC, Canada
Jaggi Rao MD FRCPC
Royal College of Physicians and Surgeons of Canada, Division of Dermatology, University of Alberta, Edmonton, AB, Canada
Jennifer Salsberg MD FRCP
Royal College of Physicians and Surgeons of Canada, University of Toronto, Women’s College Hospital, Toronto, ON, Canada, Bay Dermatology Centre, Toronto, ON, Canada Maxwell B. Sauder MD FRCPC FAAD
Royal College of Physicians and Surgeons of Canada, Dana-Farber Cancer Institute/Brigham and Women's Hospital, Boston, MA, Harvard Medical School, Boston, MA, Toronto Dermatology Centre, Toronto, ON, Canada
Catherine Zip MD FRCPC
Royal College of Physicians and Surgeons of Canada, Department of Medicine, University of Calgary, Calgary, AB, Canada, Dermatologist, Dermatology Centre, Calgary, AB, Canada
Abstract
Atopic dermatitis (AD) is a common chronic inflammatory skin disease with a prevalence of up to 25% of children and ranging from 2.1% to 4.9% of adults worldwide.
1 AD has tripled since the 1950s, now affecting 3.5% of adults in Canada and the US.
1 The dramatic increase in prevalence has occurred mainly in countries that follow a western lifestyle, and may be due to factors enhancing skin surface pH.
1
INTRODUCTION
Atopic dermatitis (AD) is a common chronic inflammatory skin disease with a prevalence of up to 25% of children and ranging from 2.1% to 4.9% of adults worldwide.1 AD has tripled since the 1950s, now affecting 3.5% of adults in Canada and the US.1 The dramatic increase in prevalence has occurred mainly in countries that follow a western lifestyle, and may be due to factors enhancing skin surface pH.1
AD presents with relapsing and remitting cycles; many AD sufferers describe being worried about the next disease exacerbation.2,3 In fact, adult patients with AD report feeling helpless (31%), anxious (40%), and irritable (31%) “quite a lot” when they think about a new disease exacerbation.3 Moreover, patients with moderate AD report having 113 days of disease exacerbation per year, while those with severe AD note having disease exacerbation more than half of the year (192 days).4
The pathogenesis of AD is multifactorial and includes genetic and environmental factors. AD presents clinically as erythematous and pruritic patches of skin with varying severity. Inflammation is believed to occur when the skin barrier becomes dysfunctional and an immune response is stimulated.5 Vice versa, the inflammatory response itself may impair the skin barrier function; once the barrier is disrupted, feedback loops are initiated.5,6 Maintaining a physiologically low skin surface pH may help to keep the skin barrier intact, reducing the risk for AD development and exacerbation of flares.
SCOPE
The current consensus paper explores the influence of genetic and environmental factors on the exacerbation of epidermal barrier breakdown in AD and to what extent these factors attribute to the elevation of stratum corneum (SC) pH. We further examine the effects of a sustained increase in skin surface pH in AD-affected skin, and explore clinical insights into the role of pH in AD. Furthermore, the influence of cleansing and moisturizer use as measure to sustain skin pH at physiological levels is also discussed.
The statements discussed in the consensus paper are intended for health care providers caring for patients with AD in pediatric and adult age groups, eg, dermatologists, pediatricians, nurses, and family physicians. Other conditions such as contact dermatitis are excluded because they have different pathogenic mechanisms.
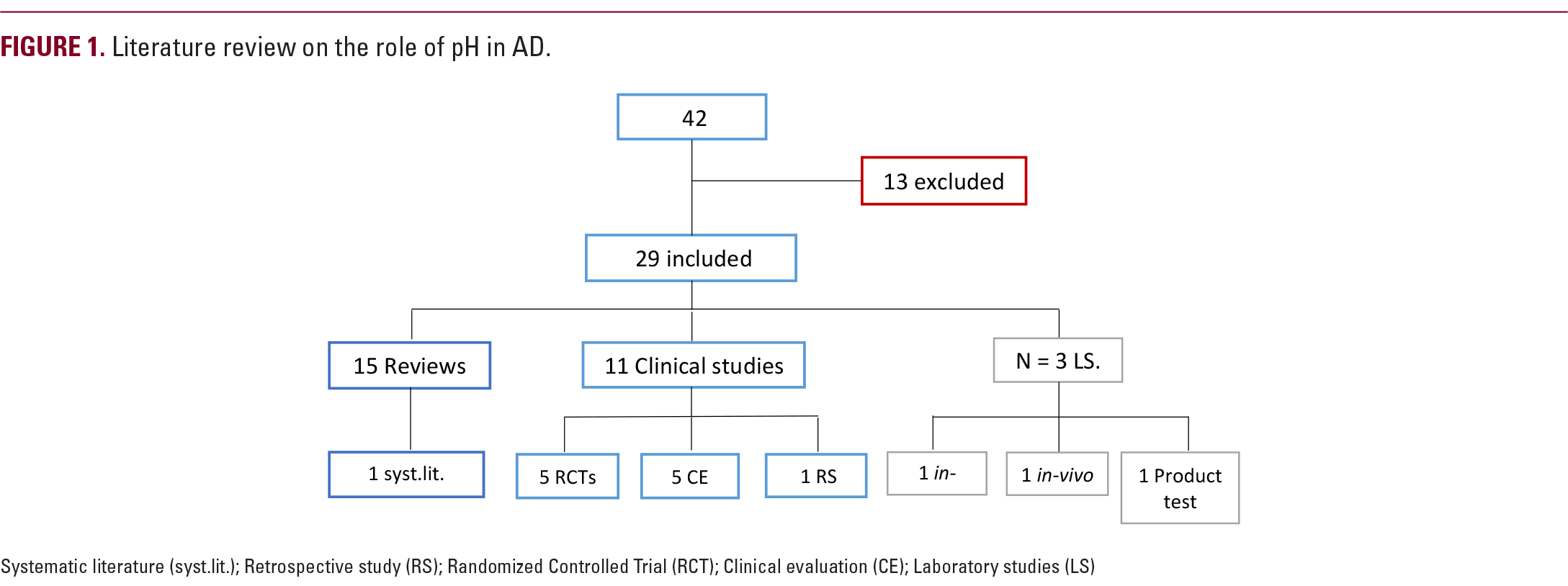
METHODS
An expert panel of dermatologists convened for a one-day meeting (January 13, 2019; Toronto, ON) to evaluate the role of skin surface pH in pediatric and adult AD populations. Additionally, they discussed the influence of cleansing and moisturizer use in these AD populations. For this purpose, evidence coupled with the expert opinion and experience of the panel was used to adopt the proposed statements and/or to add any further information or make changes. The consensus process consisted of a nominal group technique.7 Statements were developed based on the literature selected prior to the meeting; the panel then voted on the inclusion of statements after nominal group discussion.7 Consensus required a minimum of 80% agreement.