In our inclusive dermatology atlas series, we showcase side-by-side images of some of the most commonly seen dermatology conditions in an array of skin tones and briefly highlight nuances in clinical presentation. All images featured in the series are part of The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas, a resource developed by co-editors Misty Eleryan, MD, MS, and Adam Friedman, MD, and published by SanovaWorks and Educational Testing & Assessment Systems.
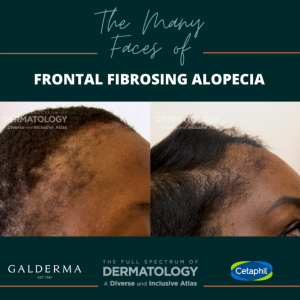
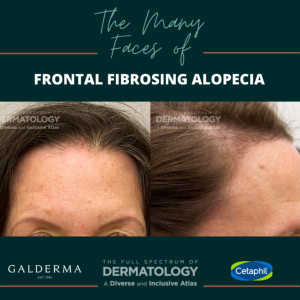
Before concluding, a patient with thinning edges has traction or androgenic alopecia, take a closer look at the scalp, face, and other hair bearing areas of the body to complete the picture. You might be missing signs and symptoms of Frontal Fibrosing Alopecia. As seen in the images, FFA can have various presentation patterns on different skin tones and hair textures.
Frontal Fibrosing Alopecia (FFA) is a cicatricial or scarring type of alopecia. It was initially categorized as a disease that only affects post-menopausal white women; however, it is now known to also affect patients of all backgrounds, skin tones, and hair textures. Though, it still most often affects females. FFA is categorized as a variant of lichen planopilaris, due to the type of lymphocytic infiltrate that attacks the hair follicles leading to permanent scarring. FFA often presents as a receding frontotemporal hairline in a band-like distribution pattern sometimes with mild erythema and perifollicular scaling. The erythema may be more difficult to visualize in darker skin types, and if present, may appear more violaceous or brown. Additionally, oils and other hair-care products that are often used in patients with more coarse/curly hair can mask the associated scale..
There is also a “lonely hair sign” that is sometimes reported with FFA and appears as one or a few isolated terminal hairs in the middle of the forehead. Small papules may also be noted on the lateral cheeks, and patients may report decreased hair growth on other parts of the body including eyebrows, extremities, axillae, and pubic regions.
Treatment of FFA should be aimed at decreasing/halting the progression of the condition using both topical and oral medications. Topical treatment includes topical and intralesional steroids as well as calcineurin inhibitors. Sometimes, patients will also incorporate topical minoxidil in addition to their other treatments. Systemic options include oral doxycycline, hydroxychloroquine, and finasteride/dutasteride as first line off label options, and immunosuppressants such as methotrexate and mycophenolate mofetil for more advanced disease. Emerging evidence supporting biologicals targeting IL-17 may prove useful. Tight hairstyles and excessive use of heat or chemicals are discouraged in patients with FFA.
Nuances to Highlight
Due the distribution pattern of FFA along the frontal hairline, diagnosis is often delayed or even missed, as it can be mistaken for androgenic alopecia, which also affects the anterior hairline in females. Also, in patients with more tightly coiled hair patterns who tend to wear higher tension hairstyles including ponytails, high buns, braids, and weave extensions, FFA can be confused with traction alopecia. Patients are also sometimes misdiagnosed with alopecia areata instead of FFA because alopecia areata can also affect the frontotemporal hairline. Also, remember that appreciable erythema or scaling of the scalp may be difficult to visualize or absent in patients with darker skin tones and tighter hair textures, so make sure to fully evaluate the scalp with a dermatoscope and always consider FFA in any patients with frontotemporal hair loss.
This article is part of Next Steps in Derm series “The Many Faces of” which showcases side-by-side images of some of the most commonly seen dermatology conditions in an array of skin tones and briefly highlight nuances in clinical presentation. All images featured in the series are part of The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas, a resource developed by co-editors Misty Eleryan, MD, MS, and Adam Friedman, MD, and published by SanovaWorks and Educational Testing & Assessment Systems.
Acknowledgements
We thank co-editors Misty Eleryan, MD, MS, and Adam Friedman, MD for reviewing the content of this article. Reposted with permission from Next Steps in Derm. Written by
Reference
Eleryan, Misty, and Adam Friedman. The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas. SanovaWorks, 2021.
NOW AVAILABLE! Visit the online image gallery for The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas, where you will find high-quality images that you will be able to use, free of charge, for non-commercial educational purposes. Access the online gallery here.