Featured Article

Successful psoriasis treatment is dependent upon accurate assessment of disease severity; however, a recent survey indicates that dermatologists report a wide variation in cutoffs for moderate disease classification on traditional quantification methods.
Successful psoriasis treatment is dependent upon accurate assessment of disease severity; however, a recent survey indicates that dermatologists report a wide variation in cutoffs for moderate disease classification on traditional quantification methods.
Successful psoriasis treatment is dependent upon accurate assessment of disease severity; however, a recent survey indicates that dermatologists report a wide variation in cutoffs for moderate disease classification on traditional quantification methods.
Due to the nature and complexity of psoriasis, authors of the survey, reported in the Journal of Drugs in Dermatology, say that a clinically useful definition of moderate plaque psoriasis is necessary to improve patient care.
“Because assessment of severity informs therapeutic decision-making, it is critical to clearly define psoriasis disease severity and offer patients therapy that is appropriate for their condition,” writes Melinda Gooderham, M.D., M.Sc., SKiN Centre for Dermatology, Ontario, Canada, who was the lead author of the report.
In the study, which is detailed in “Dermatologists’ Perspectives on Defining Moderate Psoriasis: The Canadian Moderate Psoriasis Survey,” researchers distributed a survey to 69 dermatologists asking questions about their approach to identifying and managing patients with psoriasis.
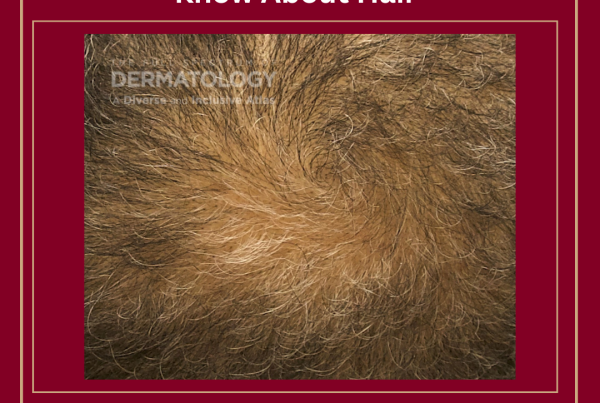
Most of the responding dermatologists reported they used the psoriasis-involved body surface area (BSA) and Psoriasis Area and Severity Index (PASI) measures to evaluate a patient’s disease severity. However, BSA has been shown to have a weak correlation with patient perception of psoriasis severity and PASI measure has a tendency to underrepresent involvement of areas such as the scalp, nail, genital and palmoplantar areas, the authors report. Therefore, these traditional measures may not adequately capture psoriasis impact on quality of life.
In using traditional classification methods, respondents reported cutoff ranges varying from 5% to 5.3% (mean) for the lower end of the BSA and 10% to 11.5% (mean) on the upper end. Similarly, the lower and upper cutoff ranges for the PASI, Dermatology Life Quality Index (DLQI) and the Physicians Global Assessment (PGA) were reported at 6 to 6.3 (mean) and 12 to 12.2 (mean), 7 to 7.3 (mean) and 11.5 to 13.0 (mean), and 2 to 2.2 and 3 to 3.2 (mean), respectively.
Dr. Palm and colleagues retrospectively reviewed the medical records of 1,002 patients who received 4,483 treatments over about 12 years to evaluate the safety of Sculptra Aesthetic at reconstitution volumes of 7-10 mL based on noted adverse events. Questionnaires were also completed by 32 injectors about their general injection procedures.
According to the review, treatments were most commonly performed in the midface/cheek, temple and jawline areas, and about half of the patients received three or four treatments during the study period. Patients averaged about 0.51-1.50 vials per treatment, which was not affected by age. All of the injectors questioned indicated they added lidocaine to their solution, which resulted in final reconstitution volumes of 8-10 mL. Mild adverse events were reported by only 36 patients (3.6%), the most common being injection site bruising and ecchymosis. Only four patients reported nodules, which were resolved with follow-up.
More than three quarters (78%) of the dermatologists in this survey estimated that less than 40% of their patients with moderate plaque psoriasis were being treated with traditional systemic therapies.
According to the authors, more than one-third of patients with psoriasis were classified as having moderate disease in the US National Psoriasis Foundation national survey data. Among patients with moderate psoriasis, more than half reported dissatisfaction with their treatment.
“Despite these efforts to classify psoriasis disease severity, psoriasis categories are often combined or collapsed for diagnostic, research, and therapeutic purposes, which may leave therapeutic needs of patients with moderate psoriasis unmet,” the authors write. “It is therefore important to clearly define this population to better understand and address their treatment goals.”
The authors write that, according to this first survey of Canadian dermatologists on moderate psoriasis, data indicate that not only is there a need to develop a more meaningful and useful definition of moderate plaque psoriasis to improve care for these patients but it also essential to raise awareness about the definition among regulatory agencies and reimbursement authorities.
Heather Onorati is an experienced medical writer and editor with more than 20 years covering the dermatology industry
Get More from the JDD
Get the latest psoriasis news delivered straight to your Inbox – sign up for the JDD Newsletter.
Discover the latest research, exclusive articles from leading dermatology experts, popular Podcast episodes, free CME activities, and more!
You May Also Like