INTRODUCTION
Hidradenitis suppurativa (HS) is an inflammatory condition characterized by recurrent abscesses and sinus tract formations in intertriginous areas of the body, which can be difficult to manage.1,2 Laser hair removal (LHR) has been shown to be an effective and safe treatment for HS.2 However, there is a paucity of data regarding dermatologists' practice patterns when using LHR for HS and their perspectives on its advantages and barriers.
MATERIALS AND METHODS
This survey-based study, approved by the Association of Academic Cosmetic Dermatology (AACD) Board, included 13 questions targeting attending physicians in both academic and private practice settings who treat HS. It captured information on LHR practices, patient characteristics, barriers to care, treatment outcomes, Hurley staging, and cost-related challenges. Responses were collected anonymously via Qualtrics and analyzed using descriptive and thematic analysis. The survey was distributed twice to AACD members and promoted at professional events (American Society for Dermatologic Surgery [ASDS] meeting and the 9th Annual Symposium of HS Advances). Additional outreach included pediatric dermatologists and residency program coordinators nationwide.
RESULTS
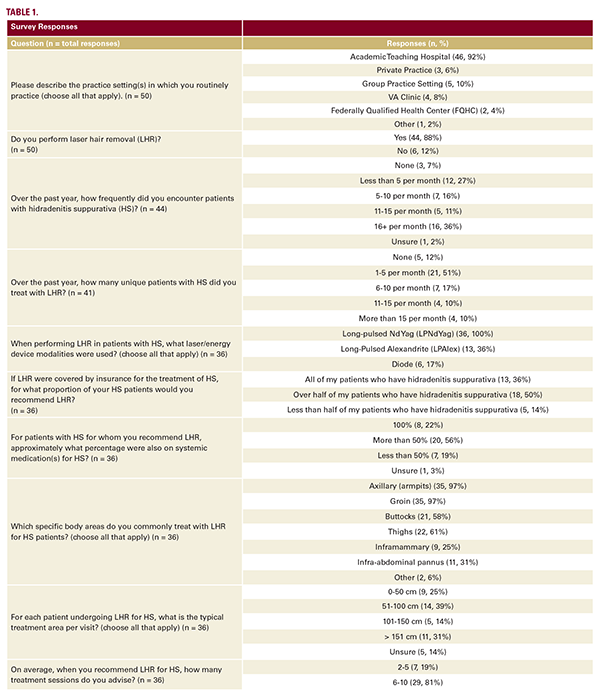
Survey results (n = 50) are outlined in Table 1. Answers to multiplechoice questions and responses to open-ended questions were quantitatively and qualitatively analyzed, respectively.
DISCUSSION
This survey of board-certified dermatologists provides valuable insights into the current practices and perceptions regarding laser hair removal (LHR) for HS treatment. The majority of respondents (88%) perform LHR, reflecting its widespread adoption in dermatology. However, the frequency of LHR use for HS varied considerably among practitioners, with 51% treating 1-5 patients per month and only 20% treating more than 10 patients monthly. This variability may reflect differences in patient populations or hesitancy to recommend LHR more broadly.
Notably, 86% of respondents would recommend LHR for over half or all of their HS patients if insurance coverage were available. Indeed, cost appears to be a significant barrier to LHR utilization, as insurance coverage and cost were frequently cited in the open-response section as challenges in determining whether or not LHR was an appropriate treatment option for HS. Lack of insurance coverage for LHR in HS management has previously been identified as a major obstacle to its widespread implementation.1
67% of dermatologists reported usually observing improvement in HS severity following LHR treatment. Furthermore, 84% of respondents feel confident or very confident in LHR's efficacy for HS management. These findings are consistent with several studies demonstrating the benefits of LHR in reducing HS severity and improving quality of life.3 Patient preferences emerged as the most influential factor (81%) in deciding to recommend or administer LHR. This patient-centered approach aligns with current recommendations for shared decisionmaking in HS management.4,5
Notably, 86% of respondents would recommend LHR for over half or all of their HS patients if insurance coverage were available. Indeed, cost appears to be a significant barrier to LHR utilization, as insurance coverage and cost were frequently cited in the open-response section as challenges in determining whether or not LHR was an appropriate treatment option for HS. Lack of insurance coverage for LHR in HS management has previously been identified as a major obstacle to its widespread implementation.1
67% of dermatologists reported usually observing improvement in HS severity following LHR treatment. Furthermore, 84% of respondents feel confident or very confident in LHR's efficacy for HS management. These findings are consistent with several studies demonstrating the benefits of LHR in reducing HS severity and improving quality of life.3 Patient preferences emerged as the most influential factor (81%) in deciding to recommend or administer LHR. This patient-centered approach aligns with current recommendations for shared decisionmaking in HS management.4,5