aspect of the right nasolabial fold. Upon examination, she was tender to palpation
along the entire length of the nasolabial fold. The overlying skin was erythematous and had a congested reticular
pattern (Figure 2b). A small amount of thick serous drainage was obtained from the
superior aspect of the right nasolabial fold. It was swabbed and sent for culture,
which returned negative for bacterial growth. The area of vascular compromise was cleansed
with betadine, and 2% nitroglycerine paste (Nitro-BID, E. Fougera & Co., Melville, NY)
was applied topically along the entire
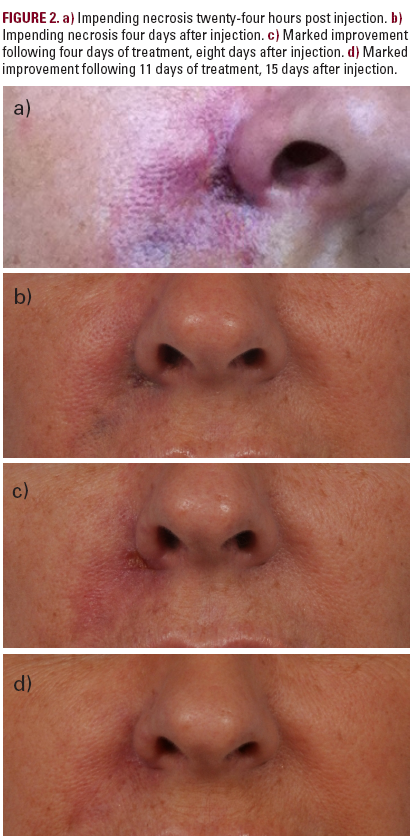
nasolabial fold, while topical antibiotic ointment was applied to the draining area.
After testing for hyaluronidase hypersensitivity,20 units of hyaluronidase (Vitrase,
ISTA Pharmaceuticals, Irvine, CA) were injected into the nasolabial fold and the patient
was started on aspirin 325 mg daily and antacids. We assumed an infectious process and
prescribed clindamycin 300 mg three times a day for seven days. The edema and erythema
continued to worsen over the next 24 hours, and levofloxacin (Levaquin, Ortho-McNeil-Janssen
Pharmaceuticals, Inc., Titusville, NJ) 750 mg daily was added to her treatment regimen.
The patient returned to our clinic four days later (Figure 2c). The area of erythema
and induration had increased to include the right upper lip; however, most of the
edema and drainage had resolved. Fifteen units of hyaluronidase were injected into
the nasolabial fold and a half inch of a 2% nitroglycerin paste was applied. The
patient was also instructed to begin placing warm compresses to the area and to
continue the antibiotics and aspirin. Application of topical oxygen infusion cream
(Dermacyte Oxygen Concentrate, Oxygen Biotherapeutics, Inc., Durham, NC) twice-daily
was begun.
After 48 hours, the induration was beginning to regress, and the area of previous drainage
and skin break down was showing signs of partial thickness epithelialization. A small amount
of crusting remained. After cleansing, a third dose of 2% nitroglycerin paste was applied to
the nasolabial fold.
One week later, upon examination, the areas of induration and erythema were nearly resolved,
and the wound at the superior aspect of the nasolabial fold had completely epithelized
(Figure 2d).Over the next several weeks, the patient returned three times for additional doses of
2% nitroglycerin paste.She believed it had an immediate effect on reducing the violaceous
reticulated color to the overlying skin. Four weeks after the initial injection, all symptoms
were resolved,and the patient was satisfied with the cosmetic improvement.
Case 3: Delayed Presentation (4 Weeks)
Patient is a 36-year-old woman with a past medical history significant for prior oral herpes infection who presented to our clinic one month after undergoing CaHA injection into her right nasolabial fold by an outside physician. Per the patient, within twenty-four hours of the injection, she noticed swelling, erythema and bruising extending from the nasolabial onto the right malar region. The wound worsened over the next several days with increasing spreading erythema and edema extending superiorly to her medial orbit and inferiorly to the inferior aspect of her nasolabial fold. There was skin breakdown and ulceration over the nasolabial fold (Figure 3a). The patient went to a local Emergency Room, where the treating physician suspected an infectious etiology. She was treated with an unknown intravenous antibiotic. A referral to a different local plastic surgeon resulted in a prescription for oral
Patient is a 36-year-old woman with a past medical history significant for prior oral herpes infection who presented to our clinic one month after undergoing CaHA injection into her right nasolabial fold by an outside physician. Per the patient, within twenty-four hours of the injection, she noticed swelling, erythema and bruising extending from the nasolabial onto the right malar region. The wound worsened over the next several days with increasing spreading erythema and edema extending superiorly to her medial orbit and inferiorly to the inferior aspect of her nasolabial fold. There was skin breakdown and ulceration over the nasolabial fold (Figure 3a). The patient went to a local Emergency Room, where the treating physician suspected an infectious etiology. She was treated with an unknown intravenous antibiotic. A referral to a different local plastic surgeon resulted in a prescription for oral






