al rates that correspond to unique genetic expression patterns.6 This classification system has been shown to work synergistically to improve prognostication when used in conjunction with previously established tools, such as the AJCC risk calculator.10 Although the ability of the test to risk-stratify patients is well established, its impact on clinician management is a newer area of study. Prior studies have demonstrated the clinical utility of a 31-GEP test on physician decision making.11,12 The effect of the results on management decisions made by physician assistants and nurse practitioners (PA/NPs), who comprise a significant portion of the dermatologic workforce, has been less studied.13 Thus, the goal of this study was to determine the impact of this technology on the management of cutaneous melanoma patients by this group.
METHODS
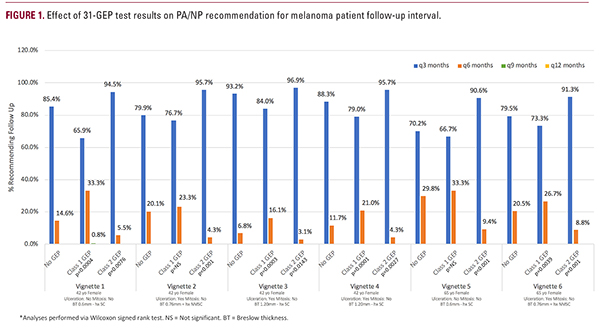
PA/NPs who attended a national dermatology conference completed an online survey with six melanoma patient vignettes. Each vignette presented patient age, gender, and history of skin cancer, along with lesion characteristics of Breslow thickness, ulceration, and presence of mitoses. Respondents answered a series of questions using pre and post-test methodology to evaluate the effect of lower and higher risk 31-GEP test results on management (decision to order SLNBx or radiologic imaging and recommended follow-up interval [q3 months, q6 months, q9 months, and q12 months]).The primary outcomes were the proportion of respondents who would alter their decision to perform a SLNBx or obtain imaging with the addition of 31-GEP test results, as well as the proportion who would alter their recommended follow-up interval. McNemar’s test was performed for assessing categorical variables, and the Wilcoxon signed rank test was performed for assessing ordinal variables. Clinical recommendations for lower and higher risk 31-GEP test results were compared to baseline (without 31-GEP test result).
RESULTS
Respondent and Patient Vignette Characteristics Overall, 164/195 (84.1% response rate) PA/NPs completed the survey. Of the respondents, 121 were PAs (73.8%) and 43 were NPs (26.2%). On average, participants reported being in dermatologic practice for 1.6 years (range, 0-4 years). Melanoma patient vignette characteristics and overall results are summarized (Table 1 and Figure 1).Impact of 31-GEP Test Results on Decision to Refer for SLNBx A lower risk 31-GEP test result led to a statistically significant decrease in the proportion of SLNBx recommended by respon-