test. For all but the thickest tumors (2.1 mm), the presence of ulceration was associated with a statistically significant increase in the proportion of respondents who would recommend the test (Table 2). For thin tumors (0.26 mm), the presence of ulceration increased the proportion of respondents who would recommend the test from a minority to a majority (22% to 67%, P<0.001). With the exception of 0.5 mm thick tumors, the presence of a SLN-negative biopsy was associated with an increased proportion of respondents who would recommend the test. However, the results were only statistically significant for 0.26 mm tumors, and even with an SLN-negative biopsy at this thickness, only a minority of clinicians would recommend the test (22% to 34%, P=0.033, Table 2).
Impact of 31-GEP Test Results on the Decision to Refer for SLNBx
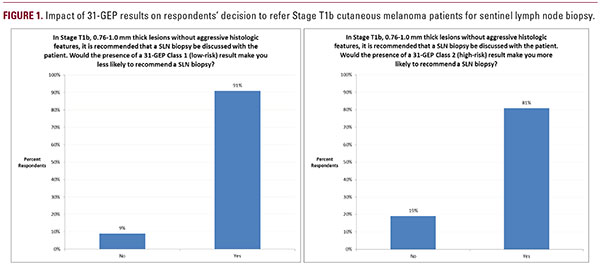
When presented a scenario in which a hypothetical patient with a Stage T1b, 0.76-1.0 mm thick melanoma underwent 31-GEP testing which returned with a Class 1 (low-risk) result, 91% of respondents reported that this result would make them less likely to recommend a SLNBx. Conversely, when the scenario was altered to reflect the same patient but with a Class 2 (high-risk) 31-GEP result, 81% of respondents stated that this result would make them more likely to recommend a SLNBx (Figure 1).
DISCUSSION
Due to the fact that the majority of melanomas are diagnosed at an early stage, a sizeable fraction of melanoma-related deaths occur in patients initially diagnosed with early-stage disease.3 Molecular diagnostics, such as the 31-GEP test, have shown potential in identifying these individuals with “low-stage” disease who have a more aggressive lesion and thus might benefit from increased intensity of management.The 31-GEP test has previously been shown to add significant prognostic value when used in combination with traditional melanoma staging methods, such as sentinel lymph node status.7 Prior work has shown that the 31-GEP test has the ability to change management in roughly half of tested patients, and that the results inform sound changes in the clinical management of melanoma.2The results of this analysis add insight into the real-world context of how clinicians use the 31-GEP test. Tumor thickness appears to play a role in the decision to order the test, with a thickness of 0.5 mm being an important cutoff. Beyond 0.5 mm of thickness, there does not appear to be significant further association between increasing thickness and likelihood of ordering the test.The presence of ulceration appears to be the most important factor considered when ordering the 31-GEP test, leading to a statistically significant increase in the proportion of clinicians who would order the test in all but the thickest tumors. For thin tumors in particular, ulceration appears to have a significant impact on clinical practice, with a majority of respondents hinging their decision to order the assay in 0.26 mm tumors on the presence of ulceration.With prior studies detailing that positive SLNBx only identifies one-third of CMM patients who experience melanoma-related mortality, one might expect a great potential for the 31-GEP test to identify high-risk lesions and possibly change management in patients with SLN-negative disease.3 Interestingly, however, SLN-negativity does not appear to be as strong of a stimulus to order the assay as ulceration. It is not surprising that SLN-negativity would have a greater impact on