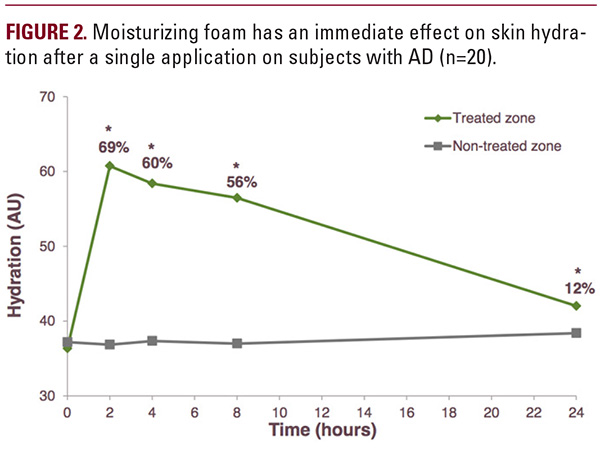
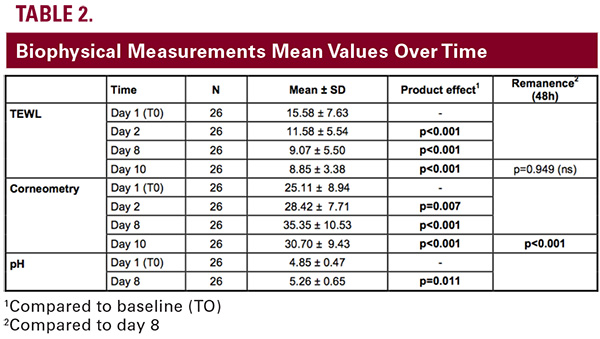
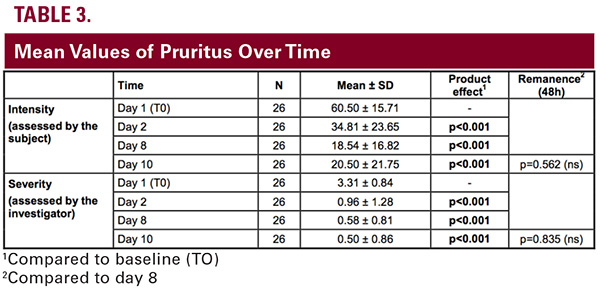
 This study was conducted to assess the effect on skin moisturizing, skin barrier regeneration, and itch relief of an anti-itch foam. The anti-itch foam was demonstrated to strengthen the skin barrier, improving TEWL and corneometry significantly after one application and throughout the longer twice-daily application period. It provided an immediate relief of clinical signs of AD, including pruritus as assessed by both the subjects and the investigators. Moreover, it delivered a long-lasting moisturizing effect, comforting of the skin, and improvement of overall skin condition.Associated itch was rapidly relieved and need to scratch significantly decreased within the first hours of the foam use. This anti-itch effect persisted for 48 hours after the last application. The early and durable anti-itch effect, the softening effect on the skin, and the cosmetic properties of the foam (easy to apply, rapidly absorbed) resulted in a 100% compliance. In this study, it was shown that a twice-daily application of the foam induced a skin moisturizing effect detected from the first 24 hours. Following a 1-week treatment period, the skin remained moisturized 48 hours after ceasing product application. The moisturizing effect as assessed by corneometry was long-lasting as it was still observed after 6 hours following a single application but faded after 24 hours, justifying an at least twice-daily regimen. Clinical scores (dryness, scaling, roughness, cracks, and scratch signs) assessed by investigators however were all significantly improved at 24 hours after a single application.Similarly, the regeneration of the skin barrier started as soon as 24 hours following the first application and this improvement was still significant 48 hours after the last product application.In conclusion, in patients with dry, sensitive, and itchy skin prone to AD, the anti-itch foam applied twice daily for 7 days proved to have a very good moisturizing effect and to be able to repair a deficient skin barrier. Associated itch was rapidly and durably relieved and need to scratch significantly decreased as well. These suggest that the anti-itch foam product may play a role in managing symptoms of AD.
This study was conducted to assess the effect on skin moisturizing, skin barrier regeneration, and itch relief of an anti-itch foam. The anti-itch foam was demonstrated to strengthen the skin barrier, improving TEWL and corneometry significantly after one application and throughout the longer twice-daily application period. It provided an immediate relief of clinical signs of AD, including pruritus as assessed by both the subjects and the investigators. Moreover, it delivered a long-lasting moisturizing effect, comforting of the skin, and improvement of overall skin condition.Associated itch was rapidly relieved and need to scratch significantly decreased within the first hours of the foam use. This anti-itch effect persisted for 48 hours after the last application. The early and durable anti-itch effect, the softening effect on the skin, and the cosmetic properties of the foam (easy to apply, rapidly absorbed) resulted in a 100% compliance. In this study, it was shown that a twice-daily application of the foam induced a skin moisturizing effect detected from the first 24 hours. Following a 1-week treatment period, the skin remained moisturized 48 hours after ceasing product application. The moisturizing effect as assessed by corneometry was long-lasting as it was still observed after 6 hours following a single application but faded after 24 hours, justifying an at least twice-daily regimen. Clinical scores (dryness, scaling, roughness, cracks, and scratch signs) assessed by investigators however were all significantly improved at 24 hours after a single application.Similarly, the regeneration of the skin barrier started as soon as 24 hours following the first application and this improvement was still significant 48 hours after the last product application.In conclusion, in patients with dry, sensitive, and itchy skin prone to AD, the anti-itch foam applied twice daily for 7 days proved to have a very good moisturizing effect and to be able to repair a deficient skin barrier. Associated itch was rapidly and durably relieved and need to scratch significantly decreased as well. These suggest that the anti-itch foam product may play a role in managing symptoms of AD. DISCLOSURES
Dr. Lio has served as a consultant/advisor and speaker for Valeant, Regeneron/Sanofi and Pierre Fabre, a consultant/advisor for Anacor, AO Biome, Exeltis, Galderma, Johnson & Johnson, Theraplex, and Mission, and has received an honrorium for his work on this supplement sponsored by Galderma.
REFERENCES
- Giam YC, Hebert AA, Dizon MV, Van Bever H, Tiongco-Recto M, Kim KH, Soebono H, Munasir Z, Diana IA, Luk DC. A review on the role of moisturizers for atopic dermatitis. Asia Pac Allergy. 2016; 6:120-128.
- Kabashima K. New concept of the pathogenesis of atopic dermatitis: interplay among the barrier, allergy, and pruritus as a trinity. J Dermatol Sci. 2013; 70:3-11.
- Vijayanand P, Seumois G, Simpson LJ, Abdul-Wajid S, Baumjohann D, Panduro M, Huang X, Interlandi J, Djuretic IM, Brown DR, Sharpe AH, Rao A, Ansel KM. Interleukin-4 production by follicular helper T cells requires the conserved Il4 enhancer hypersensitivity site V. Immunity 2012; 36:175–187.
- Zheng T, Jinho Y, Oh MH, et al. The atopic march: progression from atopic dermatitis to allergic rhinitis and asthma. Allergy Asthma Immunol Res. 2011; 3:67-73.
- Zaniboni MC, Samorano LP, Orfali RL, Aoki V. Skin barrier in atopic dermatitis: beyond filaggrin. An Bras Dermatol. 2016; 91:472-478.
- Cork MJ, Britton J, Butler L, Young S, Murphy R, Keohane SG. Comparison of parent knowledge, therapy utilization and severity of atopic eczema before and after explanation and demonstration of topical therapies by a specialist dermatology nurse. Br J Dermatol. 2003;149:582-589.
- Lindh JD, Bradley M. Clinical Effectiveness of Moisturizers in Atopic Dermatitis and Related Disorders: A Systematic Review. Am J Clin Dermatol. 2015; 16:341-359.
- Metz M, Staubach P. Itch Management: Topical Agents. Curr Probl Dermatol. 2016; 50:40-45.
- Fluhr JW, Darlenski R, Surber C. Glycerol and the skin: holistic approach to its origin and functions. Br J Dermatol. 2008;159:23-34.
- Fowler JF, Nebus J, Wallo W, Eichenfield LF. Colloidal oatmeal formulations as adjunct treatments in atopic dermatitis. J Drugs Dermatol. 2012; 11:804- 807.
- Sur R, Nigam A, Grote D, Liebel F, Southall MD. Avenanthramides, polyphenols from oats, exhibit anti-inflammatory and anti-itch activity. Arch Dermatol Res. 2008; 300:569-574.
- Schmaus G et al. Dihydroavenanthramide D for anti-irritant and anti-itch. Cosmetics and Toiletries. 2007; 122:55-66.
- Irvine AD, McLean WH. Breaking the (un)sound barrier: filaggrin is a major gene for atopic dermatitis. J Invest Dermatol. 2006; 126:1200-1202.
- Palmer CN, Irvine AD, Terron-Kwiatkowski A, et al. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nature genetics. 2006; 38:441-446.
- Howell MD, Kim BE, Gao P, Grant AV, Boguniewicz M, Debenedetto A, Schneider L, Beck LA, Barnes KC, Leung DY. Cytokine modulation of atopic dermatitis filaggrin skin expression. J Allergy Clin Immunol. 2007; 120:150- 155.
- Kamata Y, Tominaga M, Takamori K. Itch in Atopic Dermatitis Management. Curr Probl Dermatol. 2016; 50:86-93.
AUTHOR CORRESPONDENCE
Peter A. Lio MD p-lio@northwestern.edu






