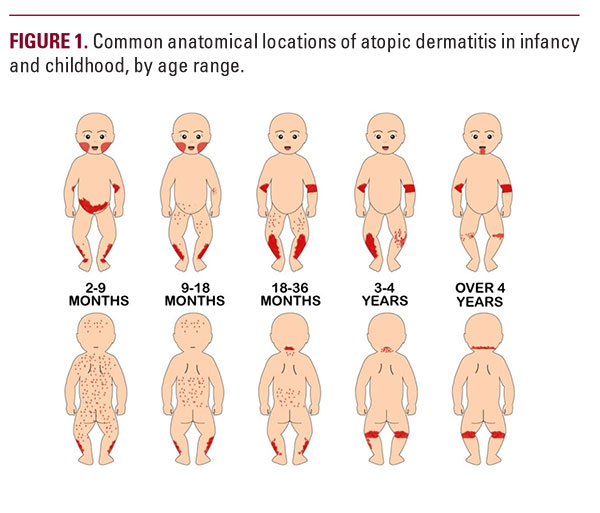
infancy, the cheeks are often affected (Figure 1), whereas in adulthood, it preferentially affects the head, neck and flexures eg, antecubital fossae, popliteal fossae.8,9 AD is associated with substantial disease-related morbidity and disability.1 Of all skin disorders, AD has the highest disability-adjusted life-years.10,11 While there are few estimates of the costs of AD, a 2002 study estimated that the direct costs to the payer were USD 3.8 billion, per year.12
AD Populations
Children are particularly at risk for developing AD. The onset of AD displays an age-dependent distribution;6 with symptoms typically appearing between two to six months of age and with 90% of atopic-prone children developing AD by the age of five years.5 The severity of AD can be classified based on symptomatology, skin lesion characteristics and the size of the affected skin area.4 Population-based survey data from the U.S. has revealed that the majority (ie, 67%) of childhood AD encompasses a mild disease state, followed by 26% and 7% of moderate and severe disease states, respectively.4,7,13 There is also evidence to suggest that individual risk factors may predispose specific individuals to AD. Notably, while there is a slight-to-no association between AD and gender,14,15 there are racial/ethnic disparities, with the severity of AD being higher in African and East Asian populations.1,16-18 Patients with AD often present with inflammatory diseases, which has led some investigators to believe that systemic immunity may predispose specific individuals.19 Given the wide variation in prevalence rates worldwide (ie, from 0.9% in India to 24.6% in Columbia), environmental factors are also thought to be involved with the development of AD.1 While research has investigated many contributing components individually, recent findings indicate that a complex interaction between the environment, host's genetics, skin barrier function, and an immune response are implicated in the development of AD.2,3
The Tri-Directional "AD-Skin Barrier-Microbiome Trinity"
AD is a multifactorial disease, with considerable individual variation with regards to the impact and combination of contributing factors.3 As such, AD has been described as a "heterogenous eczematous disorder".4 This heterogeneity contributes to the fact that the causes of AD are poorly understood. While its pathogenesis is complex, AD can be characterized by skin barrier dysfunction, aberrant immune response and dysbiosis.2 As early as the 1990s, investigators have been exploring the hypothesis that a cutaneous barrier abnormality initiates the pathogenesis of AD.3,20-22 This hypothesis followed the discovery of evidence that suggested a non-immune causative event early in the development of AD. In 2012, Kong and coworkers hypothesized that a decrease in microbial diversity and an increase in the population of staphylococcus precedes the flare of AD (Figure 2). The flared state is characterized by low bacterial diversity, consisting largely of staphylococcus. Only once diversity is increased, and the staphylococcus population normalized does the flare resolve and skin return to its baseline. Since then, the role of barrier function in AD has been investigated in numerous clinical trials.23-25 Resulting from a disruption in the skin's barrier is an increase in trans-epidermal water loss, and a decrease in skin hydration, a reduction in ceramides, fillagrin, and antimicrobial peptides. Dry and pruritic skin ensues, which prompts scratching, an exacerbation of the barrier dysfunction, and establishment of the itch-scratch cycle. Additionally, barrier dysfunction permits the penetration of external stimuli, such as allergens, toxins, irritants and bacteria which may lead to irritation, inflammation, or infection.26
While dysbiosis and barrier disruption are both components of AD, it is unclear which is the chicken and which the egg. Does the disease cause dysbiosis and barrier defect or does the aberrant stratum corneum cause atopic dermatitis? In consideration of these findings, a new concept of the pathogenesis of AD has emerged, which considers the microbiome, barrier function, and AD as an interplaying trinity.
METHODS
A working group of clinicians, all experienced in managing patient populations with AD, convened for a one-day meeting in New York City on November 2, 2019. To optimize clinical outcomes in AD, the panel reviewed literature surrounding the topic of the skin microbiome in patients with AD and developed and discussed clinical recommendations related to prevention, treatment, and maintenance of AD.
Key Insights
Cutaneous Dysbiosis in AD
Skin microbes play a critical role in maintaining skin health: controlling pathogenic species, priming the immune system, and preventing inflammation and infection. In another biinfancy,
Key Insights
Cutaneous Dysbiosis in AD
Skin microbes play a critical role in maintaining skin health: controlling pathogenic species, priming the immune system, and preventing inflammation and infection. In another biinfancy,






