Hypopigmented Mycosis Fungoides: A Clinical Mimicker of Vitiligo
February 2015 | Volume 14 | Issue 2 | Case Reports | 193 | Copyright © February 2015
Stanislav N. Tolkachjov MD and Nneka I. Comfere MD
Department of Dermatology and Laboratory Medicine and Pathology. Mayo Clinic. Rochester, MN
Abstract
Hypopigmented mycosis fungoides (HMF) is a rare variant of cutaneous T-cell lymphoma (CTCL) that often manifests in younger patients with darker skin types in a centripetal distribution.1 Average age of diagnosis is often 14 years.2 The diagnosis is often missed due to its low incidence and lack of clinical suspicion. Misdiagnosis and failure to obtain biopsies lead to a long latency period from onset of hypopigmented patches to diagnosis and treatment.
HMF has a clinically benign course and responds well to therapy; however, relapse is common.3 We report a case of HMF misdiagnosed as vitiligo in order to illuminate diagnostic, histopathological, and treatment modalities.
J Drugs Dermatol. 2015;14(2):193-194.
CASE REPORT
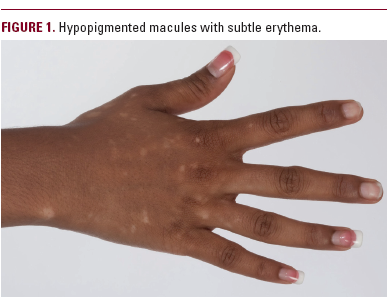
A 21-year-old woman of Fitzpatrick skin type V presents
with a 6-month history of progressive, pruritic hypopigmented
macules, without redness or scale, involving
the upper and lower extremities. She describes sparing of the
face and torso. She denies a preceding upper respiratory or
gastrointestinal infection. She does not report associated constitutional
symptoms including fevers, chills, or night sweats.
She has no prior personal or family history of dermatitis, psoriasis,
vitiligo, or autoimmunity. Prior diagnosis made by 4 local
physicians included vitiligo.
DISCUSSION